- Self Programmable Hearing Aids
- Programmable Digital Hearing Aids Prices
- Home Programmable Hearing Aids
| Hearing aid | |
|---|---|
| Other names | Deaf aid |
[edit on Wikidata] | |
- New Digital Programmable Audina Hearing aids. 2 channel open fit/over the ear hearing aid. 12 gain channels. 2 compression channels. Low Battery Indicator. NOT CHEAP SOUNDS AMPLIFIERS. PROGRAMMABLE MINI ON THE EAR RIC DIGITAL HEARING AID.
- HearSource offers the latest in discount name brand hearing aids and our proprietary personal programmable hearing aids, DIY hearing aids, self programmable hearing aids, and remote programmable hearing aids. We offer discount hearing aid repairs (on ALL brands), hearing aid batteries, hearing aid accessories and more.
- Digital hearing aids are programmable which is possible through a software. It can be programmed to a user’s hearing needs to deliver better and faster results. Though programmable analog hearing aids are also available, the digital one offers a greater degree of fine-tuning.
Self-Programmable hearing aids, no need Hipro, stand for only one digital hearing aids for wholesale channel in the digital hearing aids industry. Our AcoMate series hearing aid have obtained a great sales performance in global market.
A hearing aid is a device designed to improve hearing by making sound audible to a person with hearing loss. Hearing aids are classified as medical devices in most countries, and regulated by the respective regulations. Small audio amplifiers such as PSAPs or other plain sound reinforcing systems cannot be sold as 'hearing aids'.
Early devices, such as ear trumpets or ear horns,[1][2] were passive amplification cones designed to gather sound energy and direct it into the ear canal. Modern devices are computerised electroacoustic systems that transform environmental sound to make it audible, according to audiometrical and cognitive rules. Modern devices also utilize sophisticated digital signal processing to try and improve speech intelligibility and comfort for the user. Such signal processing includes feedback management, wide dynamic range compression, directionality, frequency lowering, and noise reduction.
Modern hearing aids require configuration to match the hearing loss, physical features, and lifestyle of the wearer. The hearing aid is fit to the most recent audiogram and is programmed by frequency. This process is called 'fitting' and is performed by a Doctor of Audiology, also called an audiologist (AuD), or by a Hearing Instrument Specialist (HIS). The amount of benefit a hearing aid delivers depends in large part on the quality of its fitting. Almost all hearing aids in use in the US are digital hearing aids.[3] Devices similar to hearing aids include the osseointegrated auditory prosthesis (formerly called the bone-anchored hearing aid) and cochlear implant.
- 3Types
- 4Technology
- 4.4Telecoil
- 4.7Processing
- 8History
- 9Regulation
- 10Cost
Uses[edit]
Hearing aids are used for a variety of pathologies including sensorineural hearing loss, conductive hearing loss, and single-sided deafness. Hearing aid candidacy is typically determined by a Doctor of Audiology, who will also fit the device based on the nature and degree of the hearing loss being treated. The amount of benefit experienced by the user of the hearing aid is multi-factorial, depending on the type, severity, and etiology of the hearing loss, the technology and fitting of the device, and on the motivation, personality, lifestyle, and overall health of the user.[4]
Hearing aids are incapable of truly correcting a hearing loss; they are an aid to make sounds more audible. The most common form of hearing loss for which hearing aids are sought is sensorineural, resulting from damage to the hair cells and synapses of the cochlea and auditory nerve. Sensorineural hearing loss reduces the sensitivity to sound, which a hearing aid can partially accommodate by making sound louder. Other decrements in auditory perception caused by sensorineural hearing loss, such as abnormal spectral and temporal processing, and which may negatively affect speech perception, are more difficult to compensate for using digital signal processing and in some cases may be exacerbated by the use of amplification.[5][page needed] Conductive hearing losses, which do not involve damage to the cochlea, tend to be better treated by hearing aids; the hearing aid is able to sufficiently amplify sound to account for the attenuation caused by the conductive component. Once the sound is able to reach the cochlea at normal or near-normal levels, the cochlea and auditory nerve are able to transmit signals to the brain normally.
Common issues with hearing aid fitting and use are the occlusion effect, loudness recruitment, and understanding speech in noise. Once a common problem, feedback is generally now well-controlled through the use of feedback management algorithms.
Candidacy and acquisition[edit]
There are several ways of evaluating how well a hearing aid compensates for hearing loss. One approach is audiometry which measures a subject's hearing levels in laboratory conditions. The threshold of audibility for various sounds and intensities is measured in a variety of conditions. Although audiometric tests may attempt to mimic real-world conditions, the patient's own every day experiences may differ. An alternative approach is self-report assessment, where the patient reports their experience with the hearing aid.[6][7]
Hearing aid outcome can be represented by three dimensions:[8]
- hearing aid usage
- aided speech recognition
- benefit/satisfaction
The most reliable method for assessing the correct adjustment of a hearing aid is through real ear measurement.[9] Real ear measurements (or probe microphone measurements) are an assessment of the characteristics of hearing aid amplification near the ear drum using a silicone probe tube microphone.[10]
Types[edit]
There are many types of hearing aids (also known as hearing instruments), which vary in size, power and circuitry.Among the different sizes and models are:
Vacuum tube hearing aid, circa 1944
Transistor body-worn hearing aid.
Pair of BTE hearing aids with earmolds.
Receiver-in-the-canal hearing aids
In-the-ear hearing aid
In-the-canal hearing aid
Completely in the canal hearing aids
Woman wearing a bone anchored hearing aid
Hearing aid application
Body-worn[edit]
Body worn aids were the first portable electronic hearing aids, and were invented by Harvey Fletcher while working at Bell Laboratories.[11] Body aids consist of a case and an earmold, attached by a wire. The case contains the electronic amplifier components, controls and battery, while the earmold typically contains a miniature loudspeaker. The case is typically about the size of a pack of playing cards and is carried in a pocket or on a belt.[12]Without the size constraints of smaller hearing devices, body worn aid designs can provide large amplification and long battery life at a lower cost. Body aids are still used in emerging markets because of their relatively low cost.[12]
Behind the ear[edit]
Behind the ear hearing aids are one of two major classes of hearing aids – Behind the ear (BTE) and In the ear (ITE). These two classes are distinguished by where the hearing aid is worn. BTE hearing aids consist of a case which hangs behind the pinna. The case is attached to an earmold or dome tip by a traditional tube, slim tube, or wire. The tube or wire courses from the superior-ventral portion of the pinna to the concha, where the ear mold or dome tip inserts into the external auditory canal. The case contains the electronics, controls, battery, and microphone(s).The loudspeaker, or receiver, may be housed in the case (traditional BTE) or in the earmold or dome tip (receiver-in-the-canal, or RIC). The RIC style of BTE hearing aid is often smaller than a traditional BTE and more commonly used in more active populations.[13]
BTEs are generally capable of providing more output and may therefore be indicated for more severe degrees of hearing loss. However, BTEs are very versatile and can be used for nearly any kind of hearing loss. BTEs come in a variety of sizes, ranging from a small, 'mini BTE,' to larger, ultra-power devices. Size typically depends on the output level needed, the location of the receiver, and the presence or absence of a telecoil. BTEs are durable, easy to repair, and often have controls and battery doors that are easier to manipulate. BTEs are also easily connected to assistive listening devices, such as FM systems and induction loops. BTEs are commonly worn by children who need a durable type of hearing aid.[12]
In the ear[edit]
In the ear aids (ITE) devices fit in the outer ear bowl (called the concha). Being larger, these are easier to insert and can hold extra features.[14] They are sometimes visible when standing face to face with someone. ITE hearing aids are custom made to fit each individual's ear. They can be used in mild to some severe hearing losses. Feedback, a squealing/whistling caused by sound (particularly high frequency sound) leaking and being amplified again, may be a problem for severe hearing losses.[15] Some modern circuits are able to provide feedback regulation or cancellation to assist with this.Venting may also cause feedback. A vent is a tube primarily placed to offer pressure equalization. However, different vent styles and sizes can be used to influence and prevent feedback.[16]Traditionally, ITEs have not been recommended for young children because their fit could not be as easily modified as the earmold for a BTE, and thus the aid had to be replaced frequently as the child grew.[17] However, there are new ITEs made from a silicone type material that mitigates the need for costly replacements.ITE hearing aids can be connected wirelessly to FM systems, for instance with a body-worn FM receiver with induction neck-loop which transmits the audio signal from the FM transmitter inductively to the telecoil inside the hearing instrument.
Mini in canal (MIC) or completely in canal (CIC) aids are generally not visible unless the viewer looks directly into the wearer's ear.[18][19] These aids are intended for mild to moderately severe losses. CICs are usually not recommended for people with good low-frequency hearing, as the occlusion effect is much more noticeable.[20] Completely-in-the-canal hearing aids fit tightly deep in the ear.[14] It is barely visible.[14] Being small, it will not have a directional microphone, and its small batteries will have a short life, and the batteries and controls may be difficult to manage.[14] Its position in the ear prevents wind noise and makes it easier to use phones without feedback.[14] In-the-canal hearing aids are placed deep in the ear canal.[14] They are barely visible.[14] Larger versions of these can have directional microphones.[14] Being in the canal, they are less likely to cause a plugged feeling.[14] These models are easier to manipulate than the smaller completely in-the-canal models but still have the drawbacks of being rather small.[14]
In-the-ear hearing aids are typically more expensive than behind-the-ear counterparts of equal functionality, because they are custom fitted to the patient's ear.In fitting, the audiologist takes a physical impression (mold) of the ear.The mold is scanned by a specialized CAD system, resulting in a 3D model of the outer ear.During modeling, the venting tube is inserted.The digitally modeled shell is printed using a rapid prototyping technique such as stereolithography.Finally, the aid is assembled and shipped to the audiologist after a quality check.[21]
Invisible in-canal hearing aids[edit]
Invisible in canal hearing aids (IIC) style of hearing aids fits inside the ear canal completely, leaving little to no trace of an installed hearing aid visible. This is because it fits deeper in the canal than other types, so that it is out of view even when looking directly into the ear bowl (concha). A comfortable fit is achieved because the shell of the aid is custom-made to the individual ear canal after taking a mold.Invisible hearing aid types use venting and their deep placement in the ear canal to give a more natural experience of hearing. Unlike other hearing aid types, with the IIC aid the majority of the ear is not blocked (occluded) by a large plastic shell. This means that sound can be collected more naturally by the shape of the ear, and can travel down into the ear canal as it would with unassisted hearing. Depending on their size, some models allow the wearer to use a mobile phone as a remote control to alter memory and volume settings, instead of taking the IIC out to do this. IIC types are most suitable for users up to middle age, but are not suitable for more elderly people.[citation needed]
Extended wear hearing aids[edit]
Extended wear hearing aids are hearing devices that are non-surgically placed in the ear canal by a hearing professional. The extended wear hearing aid represents the first 'invisible' hearing device. These devices are worn for 1–3 months at a time without removal. They are made of soft material designed to contour to each user and can be used by people with mild to moderately severe hearing loss. Their close proximity to the ear drum results in improved sound directionality and localization, reduced feedback, and improved high frequency gain.[22] While traditional BTE or ITC hearing aids require daily insertion and removal, extended wear hearing aids are worn continuously and then replaced with a new device. Users can change volume and settings without the aid of a hearing professional. The devices are very useful for active individuals because their design protects against moisture and earwax and can be worn while exercising, showering, etc. Because the device's placement within the ear canal makes them invisible to observers, extended wear hearing aids are popular with those who are self-conscious about the aesthetics of BTE or ITC hearing aid models. As with other hearing devices, compatibility is based on an individual's hearing loss, ear size and shape, medical conditions, and lifestyle. The disadvantages include regular removal and reinsertion of the device when the battery dies, inability to go underwater, earplugs when showering, and for some discomfort with the fit since it is inserted deeply in the ear canal, the only part of the body where skin rests directly on top of bone.
CROS Hearing Aid[edit]
A CROS hearing aid is a hearing aid that transmits auditory information from one side of the head to the other side of the head. Candidates include people who have poor word understanding on one side, no hearing on one side, or who are not benefiting from a hearing aid on one side. CROS hearing aids can appear very similar to behind the ear hearing aids. The CROS system can assist the patient in sound localization and understanding auditory information on their poor side.
Bone-anchored[edit]
A bone anchored hearing aid (BAHA) is a surgicallyimplantedauditoryprosthetic based on bone conduction. It is an option for patients without external ear canals, when conventional hearing aids with a mold in the ear cannot be used. The BAHA uses the skull as a pathway for sound to travel to the inner ear. For people with conductive hearing loss, the BAHA bypasses the external auditory canal and middle ear, stimulating the functioning cochlea. For people with unilateral hearing loss, the BAHA uses the skull to conduct the sound from the deaf side to the side with the functioning cochlea.
Individuals under the age of two (five in the USA) typically wear the BAHA device on a Softband. This can be worn from the age of one month as babies tend to tolerate this arrangement very well. When the child's skull bone is sufficiently thick, a titanium 'post' can be surgically embedded into the skull with a small abutment exposed outside the skin. The BAHA sound processor sits on this abutment and transmits sound vibrations to the external abutment of the titanium implant. The implant vibrates the skull and inner ear, which stimulate the nerve fibers of the inner ear, allowing hearing.
The surgical procedure is simple both for the surgeon, involving very few risks for the experienced ear surgeon. For the patient, minimal discomfort and pain is reported. Patients may experience numbness of the area around the implant as small superficial nerves in the skin are sectioned during the procedure. This often disappears after some time. There is no risk of further hearing loss due to the surgery. One important feature of the Baha is that, if a patient for whatever reason does not want to continue with the arrangement, it takes the surgeon less than a minute to remove it. The Baha does not restrict the wearer from any activities such as outdoor life, sporting activities etc.
A BAHA can be connected to an FM system by attaching a miniaturized FM receiver to it.
Two main brands manufacture BAHAs today – the original inventors Cochlear, and the hearing aid company Oticon.
Eyeglass aids[edit]
During the late 1950s through 1970s, before in-the-ear aids became common (and in an era when thick-rimmed eyeglasses were popular), people who wore both glasses and hearing aids frequently chose a type of hearing aid that was built into thetemple pieces of the spectacles.[23] However, the combination of glasses and hearing aids was inflexible: the range of frame styles was limited, and the user had to wear both hearing aids and glasses at once or wear neither.[24] Today, people who use both glasses and hearing aids can use in-the-ear types, or rest a BTE neatly alongside the arm of the glasses. There are still some specialized situations where hearing aids built into the frame of eyeglasses can be useful, such as when a person has hearing loss mainly in one ear: sound from a microphone on the 'bad' side can be sent through the frame to the side with better hearing.
This can also be achieved by using CROS or bi-CROS style hearing aids, which are now wireless in sending sound to the better side.
- Spectacle hearing aids
These are generally worn by people with a hearing loss who either prefer a more cosmetic appeal of their hearing aids by being attached to their glasses or where sound cannot be passed in the normal way, via a hearing aids, perhaps due to a blockage in the ear canal. pathway or if the client suffers from continual infections in the ear.Spectacle aids come in two forms, bone conduction spectacles and air conduction spectacles.
- Bone conduction spectacles
Sounds are transmitted via a receiver attached from the arm of the spectacles which are fitted firmly behind the boney portion of the skull at the back of the ear, (mastoid process) by means of pressure, applied on the arm of the spectacles. The sound is passed from the receiver on the arm of the spectacles to the inner ear (cochlea), via the bony portion. The process of transmitting the sound through the bone requires a great amount of power. Bone conduction aids generally have a poorer high pitch response and are therefore best used for conductive hearing losses or where it is impractical to fit standard hearing aids.
- Air conduction spectacles
Unlike the bone conduction spectacles the sound is transmitted via hearing aids which are attached to the arm or arms of the spectacles. When removing your glasses for cleaning, the hearing aids are detached at the same time. Whilst there are genuine instances where spectacle aids are a preferred choice, they may not always be the most practical option.
- Directional spectacles
These 'hearing glasses' incorporate a directional microphone capability: four microphones on each side of the frame effectively work as two directional microphones, which are able to discern between sound coming from the front and sound coming from the sides or back of the user.[25] This improves the signal-to-noise ratio by allowing for amplification of the sound coming from the front, the direction in which the user is looking, and active noise control for sounds coming from the sides or behind.Only very recently has the technology required become small enough to be fitted in the frame of the glasses. As a recent addition to the market, this new hearing aid is currently available only in the Netherlands and Belgium.[26]
Stethoscope[edit]
These hearing aids are designed for medical practitioners with hearing loss who use stethoscopes. The hearing aid is built into the speaker of the stethoscope, which amplifies the sound.
Hearing aid application[edit]
Hearing aid application (HAA) is a software which, being installed on a mobile computational platform, transforms it into a hearing aid.[27]
The principle of HAA operation corresponds to the basic principles of operation of traditional hearing aids: the microphone receives an acoustic signal and converts it into a digital form. Sound amplification is achieved by the means of a mobile computational platform, in accordance with the degree and type of users hearing loss. The processed audio signal is transformed into audio signal and output to the user into the headphones/headset. Signal processing is implemented in real time.
Constructional features of mobile computational platforms imply preferred use of stereo headsets with two speakers, which allows carrying out binaural hearing correction for the left and right ear separately.[28]HAA can work with both wired and wireless headsets and headphones.[29]
As a rule, HAA have several operation modes: setup mode and hearing aid mode. Setup mode involves the user passing an in situ-audiometry procedure, which determines the user's hearing characteristics. Hearing aid mode is a hearing correction system that corrects the user's hearing in accordance with user's hearing thresholds. HAA also incorporates background noise suppression and acoustic feedback suppression.[28]
The user can independently choose a formula to enhance the sound, as well as adjust the level of the desired amplification according to his subjective feelings.[29]
HAA have several advantages (compared to traditional hearing aids):
- the large distance between the microphone and the speaker prevents the occurrence of acoustic feedback;
- possibility to implement more convenient application control functions for people with poor motor skills;
- using of various types of headphones and headsets;
- it is possible to achieve the highest sound pressure level and get high sound quality (due to large speakers and a long battery life);
- resistant to ingress of earwax and moisture;
- it is possible to use more complex audio signal processing algorithms and a higher sampling rate (because of capacious battery);
- software flexibility;
- the set up HAA in simple cases does not require special equipment and qualifications;
- HAA does not cause any psychological inconvenience;
- the user does not need to purchase and carry any separate device.
Undoubtedly, HAA also have some disadvantages (compared to traditional hearing aids):
- more noticeable and not so comfortable to wear;
- because of the microphone is not located in the ear, it does not use the functional advantages of the auricle and the natural acoustics of the outer ear.[28]
Technology[edit]
The first electrical hearing aid used the carbon microphone of the telephone and was introduced in 1896. The vacuum tube made electronic amplification possible, but early versions of amplified hearing aids were too heavy to carry around. Miniaturization of vacuum tubes lead to portable models, and after World War II, wearable models using miniature tubes. The transistor invented in 1948 was well suited to the hearing aid application due to low power and small size; hearing aids were an early adopter of transistors. The development of integrated circuits allowed further improvement of the capabilities of wearable aids, including implementation of digital signal processing techniques and programmability for the individual user's needs.
Compatibility with telephones[edit]
A hearing aid and a telephone are 'compatible' when they can connect to each other in a way that produces clear, easily understood sound. The term 'compatibility' is applied to all three types of telephones (wired, cordless, and mobile). There are two ways telephones and hearing aids can connect with each other:
- Acoustically: the sound from the phone's speaker is picked up by the hearing aid's microphone.
- Electromagnetically: the signal inside the phone's speaker is picked up by the hearing aid's 'telecoil' or 'T-coil', a special loop of wire inside the hearing aid.
Note that telecoil coupling has nothing to do with the radio signal in a cellular or cordless phone: the audio signal picked up by the telecoil is the weak electromagnetic field that is generated by the voice coil in the phone's speaker as it pushes the speaker cone back and forth.
The electromagnetic (telecoil) mode is usually more effective than the acoustic method. This is mainly because the microphone is often automatically switched off when the hearing aid is operating in telecoil mode, so background noise is not amplified. Since there is an electronic connection to the phone, the sound is clearer and distortion is less likely. But in order for this to work, the phone has to be hearing-aid compatible. More technically, the phone's speaker has to have a voice coil that generates a relatively strong electromagnetic field. Speakers with strong voice coils are more expensive and require more energy than the tiny ones used in many modern telephones; phones with the small low-power speakers cannot couple electromagnetically with the telecoil in the hearing aid, so the hearing aid must then switch to acoustic mode. Also, many mobile phones emit high levels of electromagnetic noise that creates audible static in the hearing aid when the telecoil is used. A workaround that resolves this issue on many mobile phones is to plug a wired (not Bluetooth) headset into the mobile phone; with the headset placed near the hearing aid the phone can be held far enough away to attenuate the static. Another method is to use a 'neckloop' (which is like a portable, around-the-neck induction loop), and plug the neckloop directly into the standard audio jack (headphones jack) of a smartphone (or laptop, or stereo, etc.). Then, with the hearing aids' telecoil turned on (usually a button to press), the sound will travel directly from the phone, through the neckloop and into the hearing aids' telecoils.[30]
On 21 March 2007, the Telecommunications Industry Association issued the TIA-1083 standard,[31] which gives manufacturers of cordless telephones the ability to test their products for compatibility with most hearing aids that have a T-Coil magnetic coupling mode. With this testing, digital cordless phone manufacturers will be able to inform consumers about which products will work with their hearing aids.[32]
The American National Standards Institute (ANSI) has a ratings scale for compatibility between hearing aids and phones:
- When operating in acoustic (Microphone) mode, the ratings are from M1 (worst) to M4 (best).
- When operating in electromagnetic (Telecoil) mode, the ratings are from T1 (worst) to T4 (best).
The best possible rating is M4/T4 meaning that the phone works well in both modes. Devices rated below M3 are unsatisfactory for people with hearing aids.
Computer programs that allow the creation of a hearing aid using a PC, tablet or smartphone are currently gaining in popularity.[33] Modern mobile devices have all the necessary components to implement this: hardware (an ordinary microphone and headphones may be used) and a high-performance microprocessor that carries digital sound processing according to a given algorithm.Application configuration is carried out by the user himself in accordance with the individual features of his hearing ability. The computational power of modern mobile devices is sufficient to produce the best sound quality. This, coupled with software application settings (for example, profile selection according to a sound environment) provides for high comfort and convenience of use.In comparison with the digital hearing aid, mobile applications have the following advantages:
- ease of use (no need to use additional devices, batteries and so on.);
- high wearing comfort;
- complete invisibility (smartphone is not associated with a hearing aid);
- user-friendly interface of software settings;
- high sampling frequency (44.1 kHz) providing for excellent sound quality;
- Fast switching between the external headset and phone microphone;
- acoustic gain is up to 30 dB (with a standard headset);
- low delay in audio processing (from 6,3 to 15,7 ms – depending on the mobile device model);
- No need to get used to it, when changing mobile devices;
- No loss of settings when switching from one gadget to another and back again;
- High duration of the battery;
- free distribution of applications.
It should be clearly understood that 'hearing aid' application for smartphone / tablet cannot be considered a complete substitution of a digital hearing aid, since the latter:
- is a medical device (exposed to the relevant procedures of testing and certification);
- is designed for use by doctor's prescription;
- is adjusted using audiometry procedures.[34]
Functionality of hearing aid applications may involve a hearing test (in situ audiometry) too. However, the results of the test are used only to adjust the device for comfortable working with the application. The procedure of hearing testing in any way cannot claim to replace an audiometry test carried out by a medical specialist, so cannot be a basis for diagnosis.
- Apps such as Oticon ON for certain iOS (Apple) and Android devices can assist in locating a lost/misplaced hearing aid.[35]
Wireless[edit]
Recent hearing aids include wireless hearing aids. One hearing aid can transmit to the other side so that pressing one aid's program button simultaneously changes the other aid, so that both aids change background settings simultaneously. FM listening systems are now emerging with wireless receivers integrated with the use of hearing aids. A separate wireless microphone can be given to a partner to wear in a restaurant, in the car, during leisure time, in the shopping mall, at lectures, or during religious services. The voice is transmitted wirelessly to the hearing aids eliminating the effects of distance and background noise. FM systems have shown to give the best speech understanding in noise of all available technologies.FM systems can also be hooked up to a TV or a stereo.
2.4 gigahertz Bluetooth connectivity is the most recent innovation in wireless interfacing for hearing instruments to audio sources such as TV streamers or Bluetooth enabled mobile phones. Current hearing aids generally do not stream directly via Bluetooth but rather do so through a secondary streaming device (usually worn around the neck or in a pocket), this bluetooth enabled secondary device then streams wirelessly to the hearing aid but can only do so over a short distance. This technology can be applied to ready-to-wear devices (BTE, Mini BTE, RIE, etc.) or to custom made devices that fit directly into the ear.[36]
Oticon hearing aids for use with Bluetooth wireless devices.
Phonak wireless FM system
In developed countries FM systems are considered a cornerstone in the treatment of hearing loss in children. More and more adults discover the benefits of wireless FM systems as well, especially since transmitters with different microphone settings and Bluetooth for wireless cell phone communication have become available.[37]
Many theatres and lecture halls are now equipped with assistive listening systems that transmit the sound directly from the stage; audience members can borrow suitable receivers and hear the program without background noise. In some theatres and churches FM transmitters are available that work with the personal FM receivers of hearing instruments.
Directional microphones[edit]
Most older hearing aids have only an omnidirectional microphone. An omnidirectional microphone amplifies sounds equally from all directions. In contrast, a directional microphone amplifies sounds from one direction more than sounds from other directions. This means that sounds originating from the direction the system is steered toward are amplified more than sounds coming from other directions. If the desired speech arrives from the direction of steering and the noise is from a different direction, then compared to an omnidirectional microphone, a directional microphone provides a better signal to noise ratio. Improving the signal-to-noise ratio improves speech understanding in noise. Directional microphones have been found to be the second best method to improve the signal-to-noise ratio (the best method was an FM system, which locates the microphone near the mouth of the desired talker).[38]
Many hearing aids now have both an omnidirectional and a directional microphone mode. This is because the wearer may not need or desire the noise-reducing properties of the directional microphone in a given situation. Typically, the omnidirectional microphone mode is used in quiet listening situations (e.g. living room) whereas the directional microphone is used in noisy listening situations (e.g. restaurant). The microphone mode is typically selected manually by the wearer. Some hearing aids automatically switch the microphone mode.
Adaptive directional microphones automatically vary the direction of maximum amplification or rejection (to reduce an interfering directional sound source). The direction of amplification or rejection is varied by the hearing aid processor. The processor attempts to provide maximum amplification in the direction of the desired speech signal source or rejection in the direction of the interfering signal source. Unless the user manually temporarily switches to a 'restaurant program, forward only mode' adaptive directional microphones frequently amplify the speech of other talkers in a cocktail party type environments, such as restaurants or coffee shops. The presence of multiple speech signals makes it difficult for the processor to correctly select the desired speech signal. Another disadvantage is that some noises often contain characteristics similar to speech, making it difficult for the hearing aid processor to distinguish the speech from the noise. Despite the disadvantages, adaptive directional microphones can provide improved speech recognition in noise[39]
FM systems have been found to provide a better signal to noise ratio even at larger speaker-to-talker distances in simulated testing conditions.[40]
Telecoil[edit]
Telecoils or T-coils (from 'Telephone Coils') are small devices installed in hearing aids or cochlear implants. An Audio induction loop generates an electromagnetic field that can be detected by T-coils, allowing audio sources to be directly connected to a hearing aid. The T-coil is intended to help the wearer filter out background noise. They can be used with telephones, FM systems (with neck loops), and induction loop systems (also called 'hearing loops') that transmit sound to hearing aids from public address systems and TVs. In the UK and the Nordic countries, hearing loops are widely used in churches, shops, railway stations, and other public places. In the US, telecoils and hearing loops are gradually becoming more common. Audio induction loops, telecoils and hearing loops are gradually becoming more common also in Slovenia.
A T-coil consists of a metal core (or rod) around which ultra-fine wire is coiled. T-coils are also called induction coils because when the coil is placed in a magnetic field, an alternating electric current is induced in the wire (Ross, 2002b; Ross, 2004). Autodesk 3ds max 2014 xforce keygen 64 bits. The T-coil detects magnetic energy and transduces (converts) it to electrical energy. In the United States, the Telecommunications Industry Association's TIA-1083 standard, specifies how analog handsets can interact with telecoil devices, to ensure the optimal performance.[41]
Although T-coils are effectively a wide-band receiver, interference is unusual in most hearing loop situations. Interference can manifest as a buzzing sound, which varies in volume depending on the distance the wearer is from the source. Sources are electromagnetic fields, such as CRT computer monitors, older fluorescent lighting, some dimmer switches, many household electrical appliances and airplanes.
The states of Florida and Arizona have passed legislation that requires hearing professionals to inform patients about the usefulness of telecoils.
Legislation affecting use[edit]
In the United States, the Hearing Aid Compatibility Act of 1988 requires that the Federal Communications Commission (FCC) ensure that all telephones manufactured or imported for use in the United States after August 1989, and all 'essential' telephones, be hearing aid-compatible (through the use of a telecoil).[42]
'Essential' phones are defined as 'coin-operated telephones, telephones provided for emergency use, and other telephones frequently needed for use by persons using such hearing aids.' These might include workplace telephones, telephones in confined settings (like hospitals and nursing homes), and telephones in hotel and motel rooms. Secure telephones, as well as telephones used with public mobile and private radio services, are exempt from the HAC Act. 'Secure' phones are defined as 'telephones that are approved by the U.S. Government for the transmission of classified or sensitive voice communications.'
In 2003, the FCC adopted rules to make digital wireless telephones compatible with hearing aids and cochlear implants. Although analog wireless phones do not usually cause interference with hearing aids or cochlear implants, digital wireless phones often do because of electromagnetic energy emitted by the phone's antenna, backlight, or other components. The FCC has set a timetable for the development and sale of digital wireless telephones that are compatible with hearing aids. This effort promises to increase the number of digital wireless telephones that are hearing aid-compatible. Older generations of both cordless and mobile phones used analog technology.
Audio boot[edit]
An audio boot or audio shoe is an electronic device used with hearing aids; hearing aids often come with a special set of metal contacts for audio input. Typically the audio boot will fit around the end of the hearing aid (a behind-the-ear model, as in-the-ear do not afford any purchase for the connection) link these with another device, like an FM system or a cellphone or even a digital audio player.[43]
Direct audio input[edit]
Direct audio input (DAI) allows the hearing aid to be directly connected to an external audio source like a CD player or an assistive listening device (ALD). By its very nature, DAI is susceptible to far less electromagnetic interference, and yields a better quality audio signal as opposed to using a T-coil with standard headphones. An audio boot is a type of device that may be used to facilitate DAI.[44]
Processing[edit]
Every electronic hearing aid has at minimum a microphone, a loudspeaker (commonly called a receiver), a battery, and electronic circuitry. The electronic circuitry varies among devices, even if they are the same style. The circuitry falls into three categories based on the type of audio processing (analog or digital) and the type of control circuitry (adjustable or programmable). Hearing aid devices generally do not contain processors strong enough to process complex signal algorithms for sound source localization.[45]
Analog[edit]
Analog audio may have:
- Adjustable control: The audio circuit is analog with electronic components that can be adjusted. The hearing professional determines the gain and other specifications required for the wearer, and then adjusts the analog components either with small controls on the hearing aid itself or by having a laboratory build the hearing aid to meet those specifications. After the adjustment the resulting audio does not change any further, other than overall loudness that the wearer adjusts with a volume control. This type of circuitry is generally the least flexible. The first practical electronic hearing aid with adjustable analog audio circuitry was based on US Patent 2,017,358, 'Hearing Aid Apparatus and Amplifier' by Samual Gordon Taylor, filed in 1932.
- Programmable control: The audio circuit is analog but with additional electronic control circuitry that can be programmed by an audiologist, often with more than one program.[46] The electronic control circuitry can be fixed during manufacturing or in some cases, the hearing professional can use an external computer temporarily connected to the hearing aid to program the additional control circuitry. The wearer can change the program for different listening environments by pressing buttons either on the device itself or on a remote control or in some cases the additional control circuitry operates automatically. This type of circuitry is generally more flexible than simple adjustable controls. The first hearing aid with analog audio circuitry and automatic digital electronic control circuitry was based on US Patent 4,025,721, 'Method of and means for adaptively filtering near-stationary noise from speech' by D Graupe, GD Causey, filed in 1975. This digital electronic control circuitry was used to identify and automatically reduce noise in individual frequency channels of the analog audio circuits and was known as the Zeta Noise Blocker.
Digital[edit]
Digital audio, programmable control: Both the audio circuit and the additional control circuits are fully digital. The hearing professional programs the hearing aid with an external computer temporarily connected to the device and can adjust all processing characteristics on an individual basis. Fully digital circuitry allows implementation of many additional features not possible with analog circuitry, can be used in all styles of hearing aids and is the most flexible; for example, digital hearing aids can be programmed to amplify certain frequencies more than others, and can provide better sound quality than analog hearing aids. Fully digital hearing aids can be programmed with multiple programs that can be invoked by the wearer, or that operate automatically and adaptively. These programs reduce acoustic feedback (whistling), reduce background noise, detect and automatically accommodate different listening environments (loud vs soft, speech vs music, quiet vs noisy, etc.), control additional components such as multiple microphones to improve spatial hearing, transpose frequencies (shift high frequencies that a wearer may not hear to lower frequency regions where hearing may be better), and implement many other features. Fully digital circuitry also allows control over wireless transmission capability for both the audio and the control circuitry. Control signals in a hearing aid on one ear can be sent wirelessly to the control circuitry in the hearing aid on the opposite ear to ensure that the audio in both ears is either matched directly or that the audio contains intentional differences that mimic the differences in normal binaural hearing to preserve spatial hearing ability. Audio signals can be sent wirelessly to and from external devices through a separate module, often a small device worn like a pendant and commonly called a “streamer”, that allows wireless connection to yet other external devices. This capability allows optimal use of mobile telephones, personal music players, remote microphones and other devices. With the addition of speech recognition and internet capability in the mobile phone, the wearer has optimal communication ability in many more situations than with hearing aids alone. This growing list includes voice activated dialing, voice activated software applications either on the phone or on the internet, receipt of audio signals from databases on the phone or on internet, or audio signals from television sets or from global positioning systems. The first practical, wearable, fully digital hearing aid was invented by Maynard Engebretson, Robert E Morley, Jr. and Gerald R Popelka.[47] Their work resulted in US Patent 4,548,082, 'Hearing aids, signal supplying apparatus, systems for compensating hearing deficiencies, and methods' by A Maynard Engebretson, Robert E Morley, Jr. and Gerald R Popelka, filed in 1984. This patent formed the basis of all subsequent fully digital hearing aids from all manufacturers, including those produced currently.
The signal processing is performed by the microprocessor in real time and taking into account the individual preferences of the user (for example, increasing bass for better speech perception in noisy environments, or selective amplification of high frequencies for people with reduced sensibility to this range). The microprocessor automatically analyzes the nature of the external background noise and adapts the signal processing to the specific conditions (as well as to its change, for example, when the user goes outside from the building).[48]
Difference between digital and analog hearing aids[edit]
Analogue hearing aids make louder all the sounds picked up by the microphone. For example, speech and ambient noise will be made louder together. On the other hand, digital hearing aid (DHA) technology processes the sound using digital technology. Before transmitting the sound to the speaker, the DHA microprocessor processes the digital signal received by the microphone according to a mathematical algorithm. This allows just making louder the sounds of certain frequency according to the individual user settings (personal audiogram), and automatically adjusting the work of DHA to various environments (noisy streets, quiet room, concert hall, etc.).
For users with varying degrees of hearing loss it is difficult to perceive the entire frequency range of external sounds. DHA with multi-channel digital processing allows a user to 'compose' the output sound by fitting a whole spectrum of the input signal into it. This gives users with limited hearing abilities the opportunity to perceive the whole range of ambient sounds, despite the personal difficulties of perception of certain frequencies. Moreover, even in this 'narrow' range the DHA microprocessor is able to emphasize the desired sounds (e.g. speech), weakening the unwanted loud, high etc. sounds at the same time.
Advantages of digital aids include:According to researches[49] DHA have a number of significant advantages (compared to analoguehearing aids):
- Digital signal processing helps to reduce noise and distinguish the speech signal from the overall spectrum of sounds which facilitates speech perception.
- Reducing of background noise level increases the user's comfort (especially in noisy environments, e.g. on the street).
- Setting flexibility provides selective amplification of certain frequencies (in accordance with the personal characteristics of the hearing impaired).
- Effective acoustic feedback reduction.
- Possibility to use directional microphones, which greatly facilitates the perception of sound in certain environments, e.g., when talking face to face, or listening to the remote lecturer.
- Extended frequency range (the ability to hear a large range of sounds).
- “Self-learning' adaptive adjustment which facilitates usage of the device for a number of users.
- Possibility of connecting devices (phones, smartphones, etc.).
- In general, the maximum purification of the sound transmitted to user.
These advantages of DHA were confirmed by a number of studies,[50][51][52] relating to the comparative analysis of digital hearing aids of second and first generations and analog hearing aids.
Difference between digital hearing aid and hearing aid application[edit]
Smartphones have all the necessary hardware facilities for performing the functions of a digital hearing aid: microphone, AD converter, digital processor, DA converter, amplifier, and speakers. External microphone and speakers can also be connected as a special headset.
The operational principles of hearing aid application correspond to general operational principles of digital hearing aids: the microphone perceives an acoustic signal and converts it to digital form. Sound amplification is achieved through hardware-software means of mobile computational platform in accordance with user's hearing characteristics. Then, the signal is converted to analog form and received in the headphones by the user. The signal is processed in real time.
Taking into account the structural features of mobile computational platforms, stereo headsets with two speakers can be used, which allows to perform binaural hearing correction for the left and right ear separately.[28]
Unlike digital hearing aid, adjustment of hearing aid applications an integral part of the application itself.[29]Hearing aid application adjusted in accordance with the user's audiogram. The whole adjustment process in hearing aid application automated so that the user can perform audiometry on their own.
The hearing correction application has two modes: audiometry and correction. In the audiometry mode, hearing thresholds are measured. In the correction mode, the signal is processed with respect to the obtained thresholds.
Hearing aid applications also provides for using different computational formulas for calculation of sound amplification based on the audiometry data. These formulas are intended for maximum comfortable speech amplification and best sound intelligibility.
Hearing aid application allows saving the adjustment as different user profiles for different acoustic environments. Thus, in contrast to static settings of digital hearing aids, the user can quickly switch between the profiles depending on the change of acoustic environment.
One of the most important characteristics of the hearing aid is acoustic feedback. In hearing aid application the duration of unavoidable hardware delay is rather great, so hearing aid application uses a signal processing scheme with minimum possible algorithmic delay to make it as short as possible.[28]
Difference between PSAP and digital hearing aids[edit]
Personal Sound Amplification Products (abbreviated PSAP) are classified by the FDA as 'personal sound amplification devices.' These compact electronic devices are designed for people without hearing loss. Unlike hearing aids (which FDA classifies as devices to compensate for hearing impairment[53]) use of PSAP does not require medical prescription. Such devices are used by hunters, naturalists (for audio observation of animals or birds), ordinary people (for example, to increase the volume of the TV in a quiet room), etc.PSAP models differ significantly in price and functionality. Some devices simply amplify sound. Others contain directional microphones, equalizers to adjust the audio signal gain and filter noise.[54]
Evolution of hearing aid applications[edit]
There are audio players designed specifically for the hard-of-hearing. These applications amplify the volume of the reproduced audio signal in accordance with user's hearing characteristics and acts as music volume amplifier and assistive hearing aid. The amplification algorithm works on the frequencies that the user hears worse, thus restoring natural hearing perception of the sound of music.
Just as in hearing aid application, the player adjustment is based on the user's audiogram[55]
There are also applications that do not only adapt the sound of music to the user's hearing but also include some hearing aid functions. Such types of applications include sound amplification mode in accordance with the user's hearing characteristics as well as noise suppression mode and the mode allowing to hear the surrounding sounds without pausing the music.[56]
Jul 28, 2014 If this helped please give a thumbs up &/or support my twitch channel by giving me a follow! Link to DirectX End-User Runtime Web. Jun 10, 2012 When I open my Iso for Dolphin it says to Failed to load any D3DX9.dll update your DX9 runtime, please so ya i really dont know what to do, I looked in google but it gave me nothing. Sep 10, 2009 Vista has DX10 which is newer than DX9 however Vista uses both DX9 and DX10 and both keep getting updates every 2-3 months, the latest update by the moment of this post was November 2008 so you should update it anyway. Update dx11 runtime dolphin. The Microsoft DirectX® End-User Runtime provides updates to 9.0c and previous versions of DirectX — the core Windows® technology that drives high-speed multimedia and games on the PC. Jan 25, 2014 Try these: 0) Update to windows 8.1. Its free 1) Update drivers, Windows updates,, and latest version of Visual C++ 2) Make sure under Power Management in Windows you're running in High Performance, and are plugged in to power.
Self Programmable Hearing Aids
Also, some applications allow the hard-of-hearing watching the video and listening to the radio with comfort. Operational principles of these applications are similar to hearing aid application operational principles: the audio signal is amplified on the frequencies that the user hears worse.[57][58]
Hearing aid adaptation[edit]
It often happens that a person using a hearing aid for the first time cannot quickly make use of all its advantages.[59] Structure and characteristics of hearing aids are thoroughly devised by specialists in order to make the period of adaptation to the hearing aid as simple and quick as possible. However, despite this, a beginning hearing aid user certainly needs time to get used to it.[60]
The process of hearing prostheses consists of the following steps:[59]
- Initial adjustment of the device;
- Adaptation to new sounding;
- Fine adjustment.
Due to plasticity of central nervous system inactive hearing centers of the brain cortex switch over to processing of sound stimuli of another frequency and intensity. The brain start perceiving sounds amplified by the hearing aid right after the initial adjustment, however, it may not process them correctly at once.[59]
Feeling the hearing aid in the user's ear may seem unusual. It also takes time to adapt to the new way of hearing perception. The ear has to be gradually adjusted to the new sounding.
The sound may seem unnatural, metallic, tool loud or too quiet. Whistling sound may also appear, which is a rather unpleasant irritant.[60]
Hearing aid does not provide immediate improvement. The adaptation period can last from several hours to several months.[59]
A patient is offered a schedule of wearing their hearing aid ensuring gradual adaptation to it. If the patient starts permanently wearing the hearing aid, unfamiliar sound may cause a headache, and as a result the uses refuses to wear a hearing aid despite the fact that it helps. Surdo-teachers often run a quick preparation course for the patients. As a rule, users have inflated expectations of using hearing aids. They expect that hearing aids will help them to hear in the same way as before hearing loss, but it is not like that. Conducted trainings help hearing aid users to get accustomed to new sound feelings. A user is strongly recommended to regularly visit a surdologist, including for the purposes of additional hearing aid adjustment.[61]
Hearing aid application, in contrast to a traditional hearing aid, allows implementing nonspecific options, such as a built-in adaptation course.
The functions of the course may include:
- control over the sequence of performed exercises according to the calendar;
- control of the amount of time spent on learning (exceeding or lacking);
- reminders of daily exercises and so on.
The goal of the course is to help a user adapt to hearing aid application.
The adaptation course includes a certain number of stages, starting from listening to a set of low everyday sounds in a quiet environment, getting accustomed to one's own speech and other people's speech, getting accustomed to speech in the noise, etc.[62][63]
History[edit]
The first hearing aids were ear trumpets, and were created in the 17th century. Some of the first hearing aids were external hearing aids. External hearing aids directed sounds in front of the ear and blocked all other noises. The apparatus would fit behind or in the ear.
The movement toward modern hearing aids began with the creation of the telephone, and the first electric hearing aid, the 'akouphone,' was created about 1895 by Miller Reese Hutchison. By the late 20th century, digital hearing aids were commercially available.[64]
The invention of the carbon microphone, transmitters, digital signal processing chip or DSP, and the development of computer technology helped transform the hearing aid to its present form.[65]
History of digital aids[edit]
The history of DHA can be divided into three stages. The first stage – the widespread usage of computer simulation for the analysis of systems and algorithms for audio processing.[66] The work was conducted with the help of the 'big' computer of that time. Although they could not claim to be a real hearing aids (their performance was not enough for audio processing in real time – not to mention the size), they carried out successful studies of the various hardware circuits and algorithms for processing audio signals. The software package BLODI (stands for Block of Compiled Diagrams) developed by Kelly, Lockbaum and Vysotskiy in 1961[67] allowed to simulate any sound system provided in the form of a block diagram. With its help a special phone for users with hearing impairments was created. In 1967, Harry Levitt used BLODI to simulate a hearing aid on a digital computer.
Almost ten years later the second step was taken – the creation of 'quasi-digital' hearing aid, in which the analog components and digital programmable module was combined into a single compact case. In this device the digital controller not only controlled the analog components (amplifiers, filters and signal limiter), but it could be programmed by connecting an external computer (in the laboratory – with medical supplies of hearing aids).
The concept of quasi-digital device was very successful from a practical point of view because of the low power consumption and compact size. At that time, low-power analog amplifier technology was developed very well – in contrast to the semiconductor chips necessary for a 'real' digital camera. The combination of high performance analog components and digital signal processing capability has led to the creation module successful production parts.
Download windows 7 sp2 x64. There’s no primary distinction within the all best windows 10 but if the professional phrase is located with latest windows 10 pro then professional way there may be some further options in windows and feature the development safety of the information. you can also download For the protection and the reinforcing efficiency of your pc, you should get this windows.
The hearing aid of this type was developed by Etymonic Design. A little later, Mangold and Lane[66] created a programmable multi-channel hearing aid. A similar approach was applied by Similarly, Graupe[68] with co-authors for developing of an adaptive noise filter on a single crystal. This relatively small chip had low power consumption and fit in the case of ordinary BTE or ITC hearing aid.
The third stage of development was the appearance of 'real' digital hearing aids. In DHA all stages of sound processing are carried out in binary form. To do this, an external sound from a microphone first converted into a binary code, and after the conversion the reverse transformation is carried out (to analog signal transmitted by the ear speaker in the form of sound). The first 'real' DHA were models developed by Graup in 1970[68] on the basis of the 8080 microprocessor, which replaced the analog components (amplifier, limiter and filters). The possibilities of a programmable processor made the device self-adjusting, which opened the prospects for the use of advanced signal processing techniques, noise reduction, etc. Although the 8080th processor was relatively slow and big in size.
Further development of the DHA is associated with the creation of microprocessors with parallel processing of data arrays.[66] As a result, a significant decrease of calculations time gave the opportunity to conduct processing of audio signal in real time. The small size of microchips (as of 1987) allowed creating compact hearing aids not exceeding the dimensions of their analog 'predecessors' on their basis. However, for ITC aids these processors were not yet sufficiently compact. In all other respects, 'full' DHA of that period was very similar to modern models.
Regulation[edit]
Ireland[edit]
Like much of the Irish health care system, hearing aid provision is a mixture of public and private.
Hearing aids are provided by the State to children, OAPs and to people whose income is at or below that of the State Pension. The Irish State hearing aid provision is extremely poor; people often have to wait for two years for an appointment.
It is estimated that the total cost to the State, of supplying one hearing aid, exceeds €2,000.[citation needed]
Hearing aids are also available privately, and there is grant assistance available for insured workers. Currently for the fiscal year ending 2016, the grant stands at a maximum of €500 per ear.[69]
Irish taxpayers can also claim tax relief, at the standard rate, as hearing aids are recognised as a medical device.
Hearing aids in the Republic of Ireland are exempt from VAT.
Hearing aid providers in Ireland mostly belong to the Irish Society of Hearing Aid Audiologists.
United States[edit]
Ordinary hearing aids are Class I regulated medical devices under Federal Food and Drug Administration (FDA) rules.[70] A 1976 statute explicitly prohibits any state requirement that is 'different from, or in addition to, any requirement applicable' to regulated medical devices (which includes hearing aids) which relates 'to the safety and effectiveness of the device.'[70] Inconsistent state regulation is preempted under the federal law.[71] In the late 1970s, the FDA established federal rules governing hearing aid sales,[72] and addressed various requests by state authorities for exemptions from federal preemption, granting some and denying others.[73]
Cost[edit]
Several industrialized countries supply free or heavily discounted hearing aids through their publicly funded health care system.
Australia[edit]
The AustralianDepartment of Health and Ageing provides eligible Australian citizens and residents with a basic hearing aid free-of-charge, though recipients can pay a 'top up' charge if they wish to upgrade to a hearing aid with more or better features. Maintenance of these hearing aids and a regular supply of batteries is also provided, on payment of a small annual maintenance fee.[74]
Canada[edit]
In Canada, health care is a responsibility of the provinces. In the province of Ontario, the price of hearing aids is partially reimbursed through the Assistive Devices Program of the Ministry of Health and Long-Term Care, up to $500 for each hearing aid. Like eye appointments, audiological appointments are no longer covered through the provincial public health plan. Audiometric testing can still easily be obtained, often free of charge, in private sector hearing aid clinics and some ear, nose and throat doctors offices. Hearing aids may be covered to some extent by private insurance or in some cases through government programs such as Veterans Affairs Canada or Workplace Safety & Insurance Board.
Iceland[edit]
Social Insurance pays a one time fee of ISK 30,000 for any kind of hearing aid. However, the rules are complicated and require that both ears have a significant hearing loss in order to qualify for reimbursement. BTE hearing aids range from ISK 60,000 to ISK 300,000.[75]
India[edit]
In India hearing aids of all kinds are easily available. Under Central and state government health services, the poor can often avail themselves of free hearing devices. However, market prices vary for others and can range from Rs 1,000 to Rs 275,000 per ear.
United Kingdom[edit]
From 2000 to 2005 the Department of Health worked with Action on Hearing Loss (then called RNID) to improve the quality of NHS hearing aids so every NHS audiology department in England was fitting digital hearing aids by March 2005. By 2003 Over 175,000 NHS digital hearing aids had been fitted to 125,000 people. Private companies were recruited to enhance the capacity, and two were appointed – David Ormerod Hearing Centres, partly owned by Alliance Boots and Ultravox Group, a subsidiary of Amplifon.[76]
Within the UK, the NHS provides digital BTE hearing aids to NHS patients, on long-term loan, free of charge. Other than BAHAs (Bone anchored hearing aid), where specifically required, BTEs are usually the only style available. Private purchases may be necessary if a user desires a different style. Batteries are free.[77]
In 2014 the Clinical Commissioning Group in North Staffordshire considered proposals to end provision of free hearing aids for adults with mild to moderate age related hearing loss, which currently cost them £1.2m a year. Action on Hearing Loss mobilised a campaign against the proposal.[78]
In June 2018 the National Institute for Health and Care Excellence produced new guidance saying that hearing aids should be offered at the first opportunity after hearing loss is detected rather than waiting for arbitrary thresholds of hearing loss to be reached.[79]
United States[edit]
Most private healthcare providers in the United States do not provide coverage for hearing aids, so all costs are usually borne by the recipient. The cost for a single hearing aid can vary between $500 and $6,000 or more, depending on the level of technology and whether the clinician bundles fitting fees into the cost of the hearing aid. Though if an adult has a hearing loss which substantially limits major life activities, some state-run vocational rehabilitation programs can provide upwards of full financial assistance. Severe and profound hearing loss often falls within the 'substantially limiting' category.[80] Less expensive hearing aids can be found on the internet or mail order catalogs, but most in the under-$200 range tend to amplify the low frequencies of background noise, making it harder to hear the human voice.[81][82]
Military Veterans receiving VA medical care are eligible for hearing aids based on medical need. The Veterans Administration pays the full cost of testing and hearing aids to qualified military Veterans. Major VA medical facilities provide complete diagnostic and audiology services.[citation needed]
The cost of hearing aids is a tax-deductible medical expense for those who itemize medical deductions.[83]
Research involving more than 40,000 US households showed a convincing correlation between the degree of hearing loss and the reduction of personal income. According to the same research the tendency was not observed in almost 100% of households using DHA.[expand acronym][84]
Batteries[edit]
While there are some instances that a hearing aid uses a rechargeable battery or a long-life disposable battery, the majority of modern hearing aids use one of five standard button cellzinc–air batteries. (Older hearing aids often used mercury battery cells, but these cells have become banned in most countries today.) Modern hearing aid button cell types are typically referred to by their common number name or the color of their packaging.
They are typically loaded into the hearing aid via a rotating battery door, with the flat side (case) as the positive terminal (cathode) and the rounded side as the negative terminal (anode).
These batteries all operate from 1.35 to 1.45 volts.
The type of battery a specific hearing aid utilizes depends on the physical size allowable and the desired lifetime of the battery, which is in turn determined by the power draw of the hearing aid device. Typical battery lifetimes run between 1 and 14 days (assuming 16-hour days).
| Type/ Color Code | Dimensions (Diameter×Height) | Common Uses | Standard Names | Misc Names |
|---|---|---|---|---|
| 675 | 11.6 mm × 5.4 mm | High-Power BTEs, Cochlear Implants | IEC: PR44, ANSI: 7003ZD | 675, 675A, 675AE, 675AP, 675CA, 675CP, 675HP, 675HPX, 675 Implant Plus, 675P (HP), 675PA, 675SA, 675SP, A675, A675P, AC675, AC675E, AC675E/EZ, AC675EZ, AC-675E, AP675, B675PA, B6754, B900PA, C675, DA675, DA675H, DA675H/N, DA675N, DA675X, H675AE, L675ZA, ME9Z, P675, P675i+, PR44, PR44P, PR675, PR675H, PR675P, PR-675PA, PZ675, PZA675, R675ZA, S675A, V675, V675A, V675AT, VT675, XL675, Z675PX, ZA675, ZA675HP |
| 13 | 7.9 mm × 5.4 mm | BTEs, ITEs | IEC: PR48, ANSI: 7000ZD | 13, 13A, 13AE, 13AP, 13HP, 13HPX, 13P, 13PA, 13SA, 13ZA, A13, AC13, AC13E, AC13E/EZ, AC13EZ, AC-13E, AP13, B13BA, B0134, B26PA, CP48, DA13, DA13H, DA13H/N, DA13N, DA13X, E13E, L13ZA, ME8Z, P13, PR13, PR13H, PR-13PA, PZ13, PZA13, R13ZA, S13A, V13A, VT13, V13AT, W13ZA, XL13, ZA13 |
| 312 | 7.9 mm × 3.6 mm | miniBTEs, RICs, ITCs | IEC: PR41, ANSI: 7002ZD | 312, 312A, 312AE, 312AP, 312HP, 312HPX, 312P, 312PA, 312SA, 312ZA, AC312, AC312E, AC312E/EZ, AC312EZ, AC-312E, AP312, B312BA, B3124, B347PA, CP41, DA312, DA312H, DA312H/N, DA312N, DA312X, E312E, H312AE, L312ZA, ME7Z, P312, PR312, PR312H, PR-312PA, PZ312, PZA312, R312ZA, S312A, V312A, V312AT, VT312, W312ZA, XL312, ZA312 |
| 10 | 5.8 mm × 3.6 mm | CICs, RICs | IEC: PR70, ANSI: 7005ZD | 10, 10A, 10AE, 10AP, 10DS, 10HP, 10HPX, 10SA, 10UP, 20PA, 230, 230E, 230EZ, 230HPX, AC10, AC10EZ, AC10/230, AC10/230E, AC10/230EZ, AC230, AC230E, AC230E/EZ, AC230EZ, AC-230E, AP10, B0104, B20BA, B20PA, CP35, DA10, DA10H, DA10H/N, DA10N, DA230, DA230/10, L10ZA, ME10Z, P10, PR10, PR10H, PR230H, PR536, PR-10PA, PR-230PA, PZA230, R10ZA, S10A, V10, VT10, V10AT, V10HP, V230AT, W10ZA, XL10, ZA10 |
| 5 | 5.8 mm × 2.1 mm | CICs | IEC: PR63, ANSI: 7012ZD | 5A, 5AE, 5HPX, 5SA, AC5, AC5E, AP5, B7PA, CP63, CP521, L5ZA, ME5Z, P5, PR5H, PR-5PA, PR521, R5ZA, S5A, V5AT, VT5, XL5, ZA5 |
See also[edit]
- El Deafo (Cece Bell novel)
- Orkney Wireless Museum – has a 1930s Ardent hearing aid in its collection
- Sonotone 1010 – first electronic hearing aid to use a transistor
References[edit]
- ^Bentler Ruth A., Duve, Monica R. (2000). 'Comparison of Hearing Aids Over the 20th Century'. Ear & Hearing. 21 (6): 625–639. doi:10.1097/00003446-200012000-00009.CS1 maint: Multiple names: authors list (link)
- ^'Ear Horn Q&A'. Archived from the original on 24 July 2008. Retrieved 6 December 2007.
- ^Kochkin, Sergei (January 2010). 'Sergei Kochkin – MarkeTrak VIII: Consumer satisfaction with hearing aids is slowly increasing'. The Hearing Journal. journals.lww.com. 63 (1): 19. doi:10.1097/01.HJ.0000366912.40173.76. Retrieved 18 February 2015.
- ^Robyn M Cox, Jani A Johnson, and Jingjing Xu (1 July 2017). 'Impact of Hearing Aid Technology on Outcomes in Daily Life I: the Patients' Perspective'. Ear Hear. 37 (4): e224–37. doi:10.1097/AUD.0000000000000277. PMC4925253. PMID26881981.CS1 maint: Multiple names: authors list (link)
- ^J., Moore, Brian C. (2007). Cochlear hearing loss : physiological, psychological and technical issues (2nd ed.). Chichester: John Wiley & Sons. ISBN9780470516331. OCLC180765972.
- ^Bentler, R. A.; Kramer, S. E. (2000). 'Guidelines for choosing a self-report outcome measure'. Ear and Hearing. 21 (4 Suppl): 37S–49S. doi:10.1097/00003446-200008001-00006. PMID10981593.
- ^Taylor, Brian (22 October 2007). 'Self-Report Assessment of Hearing Aid Outcome – An Overview'. AudiologyOnline. Archived from the original on 29 January 2015. Retrieved 29 May 2013.
- ^Humes, Larry E. and Humes, Lauren E. (2004). 'Factors Affecting Long-Term Hearing Aid Success'. Seminars in Hearing. 25 (1): 63–72. doi:10.1055/s-2004-823048.CS1 maint: Multiple names: authors list (link)
- ^Katz, Jack; Medwetsky, Larry; Burkard, Robert; Hood, Linda (2009). 'Chapter 38, Hearing Aid Fitting for Adults: Selection, Fitting, Verification, and Validation'. Handbook of Clinical Audiology (6th ed.). Baltimore MD: Lippincott Williams & Wilkins. p. 858. ISBN978-0-7817-8106-0.
- ^Stach, Brad (2003). Comprehensive Dictionary of Audiology (2nd ed.). Clifton Park NY: Thompson Delmar Learning. p. 167. ISBN978-1-4018-4826-2.
- ^Hartmann, William M. (14 September 2004). Signals, Sound, and Sensation. Springer Science & Business Media. pp. 72–. ISBN978-1-56396-283-7. Archived from the original on 3 December 2016.
- ^ abcHearing Aid Basics, National Institute of Health, archived from the original on 13 November 2011, retrieved 2 December 2011
- ^'Hearing Aids'. National Institute on Deafness and Other Communication Disorders. Archived from the original on 15 September 2012. Retrieved 9 September 2012.
- ^ abcdefghij'Hearing Aid Buying Guide'. Consumer Reports. February 2017. Archived from the original on 12 February 2017. Retrieved 13 February 2017.
- ^'Problems with hearing aids: Ask our audiologist – Action On Hearing Loss: RNID'. Action On Hearing Loss. Archived from the original on 17 June 2016. Retrieved 28 December 2016.
- ^Sickel, K. (13 September 2007) Shortest Path Search with Constraints on Surface Models of In-ear Hearing Aids52. IWK, Internationales Wissenschaftliches Kolloquium (Computer science meets automation Ilmenau 10.) Vol. 2 Ilmenau : TU Ilmenau Universitätsbibliothek 2007, pp. 221–226
- ^'Hearing Aids for Children'. Hearing Aids for Children. American Speech-Language-Hearing Association. Retrieved 1 December 2014.
- ^Eisenberg, Anne (24 September 2005) The Hearing Aid as Fashion StatementArchived 6 January 2016 at the Wayback Machine. NY Times.
- ^Dybala, Paul (6 March 2006) ELVAS Sightings – Hearing Aid or HeadsetArchived 16 August 2012 at the Wayback Machine. AudiologyOnline.com.
- ^Ross, Mark (January 2004) The 'Occlusion Effect' – What it is, and What to Do About itArchived 15 February 2016 at the Wayback Machine, hearingresearch.org.
- ^Sickel, K. et al. (2009) 'Semi-Automatic Manufacturing of Customized Hearing Aids Using a Feature Driven Rule-based Framework'. Proceedings of the Vision, Modeling, and Visualization Workshop 2009 (Braunschweig, Germany 16–18 November 2009), pp. 305–312
- ^Sanford, Mark J., MS; Anderson, Tamara; Sanford, Christine (10 March 2014). 'The Extended-Wear Hearing Device: Observations on Patient Experiences and Its Integration into a Practice'. The Hearing Review. 24 (3): 26–31. Archived from the original on 5 December 2014. Retrieved 1 December 2014.
- ^'Concealed Hearing Devices of the 20th Century'. Concealed Hearing Devices of the 20th Century. Bernard Becker Medical Library. Archived from the original on 23 January 2015. Retrieved 1 December 2014.
- ^'Why Don't They Made Hearing Aids Glasses Anymore'. www.hearreview.com. Retrieved 27 November 2018.
- ^Netherlands: Dutch Unveil 'Varibel' – The Eyeglasses That HearArchived 15 April 2012 at the Wayback Machine, Publish Date: 1 March 2007, Related Company Website: www, varibel.nl. Accessed 10 February 2008.
- ^The manufacturer's website is published in Dutch and French at 'Archived copy'. Archived from the original on 22 February 2008. Retrieved 9 February 2016.CS1 maint: Archived copy as title (link) and there is a TV news report in English at http://varibel.nl/site/Files/default.asp?iChannel=4&nChannel=FilesArchived 22 February 2008 at the Wayback Machine
- ^'Mobile Medical Applications. Guidance for Industry and Food and Drug Administration Staff'(PDF). Food and Drug Administration. 2015.
- ^ abcdeE.S. Azarov, M.I. Vashkevich, S.V. Kozlova, A.A. Petrovsky (2014). 'Hearing correction system based on mobile computing platform (in Russian)'. Informatics. 2 (42): 5–24. ISSN1816-0301.CS1 maint: Multiple names: authors list (link)
- ^ abcA. Vonlanthen, H. Arndt (2009). Hearing aids (in Russian). Translated by T. Gvelesiani. Rostov-on-Don: Feniks. ISBN978-5-222-15490-8.
- ^Mestayer, Kathi. 'Staff Writer'. Hearing Health Magazine. Archived from the original on 22 February 2014. Retrieved 13 February 2014.
- ^TIA-1083 Revision A, November 17, 2010Archived 16 May 2012 at the Wayback Machine. ihs.com
- ^'New TIA Standard Will Improve Hearing Aid Compatibility with Digital Cordless Phones'. U.S. Telecommunications Industry Association. 5 April 2007. Archived from the original on 6 December 2010. Retrieved 3 November 2011.
- ^'Приложение для смартфонов заменит глухим слуховой аппарат? – Глухих.нет. Новостной портал для глухих и слабослышащих | Новости мира глухих и слабослышащих | Сайт глухих | Спорт глухих | Can application substitute hearing aid?'. gluxix.net. 13 March 2014. Retrieved 18 February 2015.
- ^'Mobile Medical Applications'. fda.gov. Retrieved 18 February 2015.
- ^http://www.oticon.global/solutions/accessories/connectivity, Retrieved 2016-09-25.
- ^Mroz, Mandy. 'Hearing Aids and Bluetooth Technology'. Hearing Aids and Bluetooth Technology. Healthy Hearing. Archived from the original on 9 November 2014. Retrieved 1 December 2014.
- ^Dave Fabry; Hans Mülder; Evert Dijkstra (November 2007). 'Acceptance of the wireless microphone as a hearing aid accessory for adults'. The Hearing Journal. 60 (11): 32–36. doi:10.1097/01.hj.0000299170.11367.24.
- ^Hawkins D (1984). 'Comparisons of speech recognition in noise by mildly-to-moderately hearing-impaired children using hearing aids and FM systems'. Journal of Speech and Hearing Disorders. 49 (4): 409. doi:10.1044/jshd.4904.409.
- ^Ricketts T.; Henry P. (2002). 'Evaluation of an adaptive, directional-microphone hearing aid'. International Journal of Audiology. 41 (2): 100–112. doi:10.3109/14992020209090400.
- ^Lewis, M. Samantha; Crandell, Carl C.; Valente, Michael; Horn, Jane Enrietto (2004). 'Speech perception in noise: directional microphones versus frequency modulation (FM) systems'. Journal of the American Academy of Audiology. 15 (6): 426–439. doi:10.3766/jaaa.15.6.4.
- ^TIA-1083: A NEW STANDARD TO IMPROVE CORDLESS PHONE USE FOR HEARING AID WEARERSArchived 25 April 2012 at the Wayback Machine. U.S. Telecommunications Industry Association
- ^'Public Law 100-394, [47 USC 610] – Hearing Aid Compatibility Act of 1988'. PRATP. Archived from the original on 26 July 2010. Retrieved 8 June 2013.
- ^'Boot Definition'. www.nchearingloss.org. Retrieved 2 June 2017.
- ^'Boot Definition'. www.nchearingloss.org. Archived from the original on 3 March 2016. Retrieved 2 June 2017.
- ^Ganguly Anshuman, Reddy Chandan, Hao Yiya, Panahi Issa (2016). Improving Sound Localization for Hearing Aid Devices Using Smartphone Assisted Technology. 2016 IEEE International Workshop on Signal Processing Systems (SiPS). pp. 165–170. doi:10.1109/SiPS.2016.37. ISBN978-1-5090-3361-4.CS1 maint: Multiple names: authors list (link)
- ^Heidtman, Laurel (28 September 2010). 'Analog Vs. Digital Hearing Aids'. LiveStrong.com. Archived from the original on 3 May 2012. Retrieved 23 July 2012.
- ^Levitt, Harry (26 December 2007). 'Digital Hearing Aids'. The Asha Leader. Archived from the original on 17 July 2012. Retrieved 23 July 2012.
- ^'Как работают слуховые аппараты'. radugazvukov.ru. Archived from the original on 25 December 2014. Retrieved 18 February 2015.
- ^Janet McCaffrey (21 December 2009). 'HJ0905 Kochkin copy'(PDF). The Hearing Journal. Retrieved 18 February 2015.
- ^'Fitting Tips: Essentials of Hearing Aid Selection, Part 1: Cosmetics Are Not Just What Meets the Ear – Hearing Review'. hearingreview.com. Retrieved 18 February 2015.
- ^Richard Preid Fotorotar AG (8 August 2007). '24_P54090_Pho_Kapitel_06bis07'(PDF). Retrieved 18 February 2015.
- ^'Hearing Review Three-Year Index 2003–2005 – Hearing Review'. hearingreview.com. Retrieved 18 February 2015.
- ^'Применение технологии широкополосного изменения огибающей спектра звукового сигнала Petralex® в онлайн-приложениях коррекции слуха::Журнал СА 7–8.2014 (Mann, Eric A., M.D., Ph.D., 'Hearing Aids and Personal Sound Amplifiers: Know the Difference', U.S. Food and Drug Administration Consumer Updates website, Oct. 20, 2009. Retrieved 2013-05-23.)'. samag.ru. Retrieved 18 February 2015.
- ^Beck, Melinda, “Getting an Earful: Testing A Tiny, Pricey Hearing Aid”, The Wall Street Journal, Jan. 29, 2008. Retrieved 2013-05-23.
- ^'Music Volume Booster'. App Store. Retrieved 28 May 2019.
- ^'UrbanDenoiser Player'. App Store. Retrieved 28 May 2019.
- ^'Youtube Volume Booster'. App Store. Retrieved 28 May 2019.
- ^'Radio Volume Booster'. App Store. Retrieved 28 May 2019.
- ^ abcd'Адаптация к слуховому аппарату'. r-sluh.ru. Retrieved 28 May 2019.
- ^ ab'Адаптация к слуховому аппарату'. www.xn----ttbbfjpems.xn—p1ai. Retrieved 28 May 2019.
- ^Королева, Инна Васильевна (2012). Введение в аудиологию и слухопротезирование (in Russian). КАРО. ISBN9785992507379.
- ^'Free apps help better hearing!'. PETRALEX Hearing Aid. Retrieved 28 May 2019.
- ^'Petralex Hearing Aid App'. App Store. Retrieved 28 May 2019.
- ^Mills, Mara (2011). 'Hearing Aids and the History of Electronics Miniaturization'. IEEE Annals of the History of Computing. 33 (2): 24–45. doi:10.1109/MAHC.2011.43.
- ^Howard, Alexander (26 November 1998). 'Hearing Aids: Smaller and Smarter.'Archived 28 December 2016 at the Wayback MachineNew York Times.
- ^ abc'LEVITT: Digital Hearing Aids: A Tutorial Review'(PDF). rehab.research.va.gov. Retrieved 18 February 2015.
- ^Kelly LJ, Jr.; Lochbaum C; Vyssotsky VA. A block diagram compiler. Bell System Tech J (40):669–676, 1961.
- ^ abGraupe D, Grosspietsch JK, Basseas SP. 'A single microphone-based self-adaptive filter of noise from speech and its performance evaluation. J Rehabil Res Dev 24(4), 1987 (this issue'(PDF). rehab.research.va.gov. Retrieved 18 February 2015.
- ^'Aural'. Ireland Department of Social Protection. Archived from the original on 2 July 2012. Retrieved 23 July 2012.
- ^ ab21 U.S.C.§ 360k (a) (2005).
- ^Missouri Board of Examiners for Hearing Instrument Specialists v. Hearing Help Express, Inc., 447 3d 1033 (8th Cir. 2006)
- ^Final Rule issued in Docket 76N-0019, 42 FR9286 (15 February 1977).
- ^Exemption from Preemption of State and Local Hearing Aid Requirements; Applications for Exemption, Docket No. 77N-0333, 45 FR67326; Medical Devices: Applications for Exemption from Federal Preemption of State and Local hearing Aid Requirements, Docket No. 78P-0222, 45 FR67325 (10 October 1980).
- ^'Understanding the Australian Government Hearing Services Program'. Archived from the original on 9 September 2007. Retrieved 4 December 2007.
- ^Social Insurance Administration – Iceland Accessed 30 November 2007 Archived 16 February 2008 at the Wayback Machine
- ^'Loud and clear'. Health Service Journal. 18 December 2003. Archived from the original on 23 October 2014. Retrieved 17 October 2014.
- ^NHS hearing aid service fact sheet Accessed 26 November 2007 Archived 2 October 2010 at the Wayback Machine
- ^'Hearing aid charging opposed in feedback exercise'. Health Service Journal. 23 September 2014. Archived from the original on 9 October 2014. Retrieved 17 October 2014.
- ^'Doctors should prescribe hearing aids at first sign that hearing loss is affecting life'. Daily Mail. 21 June 2018. Retrieved 21 June 2018.
- ^'Questions and Answers about Deafness and Hearing Impairments in the Workplace and the Americans with Disabilities Act'. U.S. Equal Employment Opportunity Commission. Archived from the original on 4 March 2016. Retrieved 26 November 2007.
- ^Mahany, Barbara (9 March 2011). 'Now Hear This'. Chicago Tribune. Archived from the original on 15 June 2013.
- ^Romano, Tricia (22 October 2012). 'The Hunt for an Affordable Hearing Aid'. Well. New York Times. Archived from the original on 25 February 2015.
- ^'Topic 502 – Medical and Dental Expenses'. Internal Revenue Service. Archived from the original on 3 July 2017. Retrieved 26 November 2007.
- ^Kochkin, Sergei (October 2010). 'MarkeTrak VIII: The efficacy of hearing aids in achieving compensation equity in the workplace'. The Hearing Journal. 63 (10): 19–24, 26, 28. doi:10.1097/01.HJ.0000389923.80044.e6. Retrieved 18 February 2015.
External links[edit]
| Wikimedia Commons has media related to Hearing aids. |
- Information from the National Institutes of Health (NIH)
- American Hearing Research Foundation funds research in hearing and aims to help educate the public in the United States.
- Royal National Institute for Deaf Information and resources about hearing loss.
- Historical
Abstract
The need for reliable access to hearing health care services is growing globally, particularly in developing countries and in remotely located, underserved regions in many parts of the developed world. Individuals with hearing loss in these areas are at a significant disadvantage due to the scarcity of local hearing health care professionals and the high cost of hearing aids. Current approaches to making hearing rehabilitation services more readily available to underserved populations include teleaudiology and the provision of amplification devices outside of the traditional provider-client relationship. Both strategies require access to such resources as dedicated equipment and/or specially trained staff. Another possible strategy is a self-fitting hearing aid, a personal amplification device that is equipped with an onboard tone generator to enable user-controlled, automated, in situ audiometry; an onboard prescription to determine the initial hearing aid settings; and a trainable algorithm to enable user-controlled fine-tuning. The device is thus assembled, fitted, and managed by the user without the need for audiological or computer support. This article details the self-fitting concept and its potential application in both developing and developed countries. Potential advantages and disadvantages of such a device are discussed, and considerations for further investigations into the concept are presented. Overall, the concept is considered technologically viable with the main challenges anticipated to be development of clear, simple user instructions and a delivery model that ensures reliable supplies of instant-fit ear tips and batteries.
Background
Of the 278 million people in the world with bilateral, moderate to profound hearing loss, two-thirds live in developing countries (WHO, 2004). Although there are no formally established criteria for the designation of countries as “developing,” the United Nations Conference on Trade and Development (UNCTAD) groups economically disadvantaged countries according to three categories, across which there is some overlap: least developed countries (LDC), small island developing states (SIDS), and land-locked developing countries (LLDC). Nations belonging to these categories are characterized by low per capita gross national income (GNI), high child mortality rates, low adult literacy rates, and political and economic instability (UN-OHRLLS, 2010). For the purposes of this article, we define a “developing country” as a nation that belongs to at least one of the above three categories. Based on this definition, such countries as Angola, Myanmar, and Haiti are considered developing countries.
Of those individuals in developing countries who have a permanent bilateral hearing loss of moderate degree or greater, approximately three-quarters have adult-onset hearing loss, the third leading cause of disability in the world (Smith, 2008). Most of the 186 million hearing-impaired people in developing countries could benefit from amplification, but current annual production and distribution of hearing aids is estimated to meet less than 3% of the need in this part of the world (WHO, 2004). One of the many barriers to accessing hearing aids in developing countries is cost. The World Health Organization (WHO) has established global guidelines for hearing aid affordability that vary according to each country’s per capita GNI, thus relating hearing aid expenditure to average household income. The WHO guidelines suggest that a single hearing aid should not exceed 3% of per capita GNI. For example, in a country with a per capita GNI of US$45,000, WHO guidelines stipulate that a hearing aid should cost approximately US$1,300, whereas in a developing country with a per capita GNI of US$550, the cost of the device should not exceed US$10 (Brouillette, 2008). Other researchers have stressed the requirement that devices for developing countries be made affordable to as many residents as possible (e.g., ; ).
Another barrier to hearing aid rehabilitation in developing countries is a deficit of skilled hearing health care professionals. In developing countries, the proportion of audiologists ranges from 1 per 500,000 to 1 per 6,250,000 people (Goulios & Patuzzi, 2008). Further, approximately 20% of the countries surveyed by Goulios and Patuzzi (2008), all of which had very low per capita GNI, reported having no audiologists at all. Currently, many developing countries receive hearing health care through local general practitioners and/or teachers of the deaf, as well as visiting aid agencies. However, many charitable organizations who visit developing countries do not leave behind a self-sustaining infrastructure. A case study reported in McPherson (2008) describes the occurrence of such a situation in The Gambia, an LDC in which an audiology clinic was established with the support of British and Scandinavian aid agencies. The clinic employed two trained staff members, both of whom subsequently left the area and caused the clinic’s closure after only a few years. Staff transience is a particular problem in the audiology field as there are more jobs than there are qualified people to fill them. Audiologists from developing countries, seeking to improve their own socioeconomic situation, will often migrate to fill positions in developed countries, thus creating chronic personnel shortages in their home country. Other contributors to the closure of the Gambian clinic included the high cost of purchasing equipment, a lack of local calibration and repair facilities, and the high cost of sending equipment overseas for these services (McPherson, 2008).
To address the significant shortage of clinical skills in developing countries, the viability of teleaudiology is being explored. provides an excellent introduction to teleaudiology and the potential scope of its applications. Briefly, teleaudiology refers to the practice of audiology in which the clinician is situated remotely from the client and delivers services via information and communication technology, such as the telephone or internet. Teleaudiology has been successfully trialed for diagnostic testing (e.g., ; ), hearing aid adjustment (e.g., Ferrari, 2006; ), and counseling (e.g., ; Pearce, Ching, & Dillon, 2009). There is no doubt that technological advancement and the penetration of communication technologies into developing countries make teleaudiology a very viable strategy. , however, have pointed out that such potential complications as licensure, jurisdictional responsibility, certification, reimbursement, and quality control need to be addressed, as clinicians and clients could potentially be situated in different states or even in different countries. Further, the establishment of a teleaudiology network still requires resources, including specialized equipment and dedicated local staff to assist the client, obtain information, and/or to guide the process. The introduction of teleaudiology could also place undue burden on clinicians in developed countries, where staff shortages also exist, if they are tapped to provide remote services to clients in developing countries.
Even among individuals with hearing impairment in developed nations who have reliable access to hearing health care services, the majority do not acquire hearing aids. Only about one in five individuals with hearing impairment in the developed world have obtained hearing aids, a number that has not substantially changed in 30 years (Dillon, in press; Kochkin, 2005). The reasons for the low penetration rate are varied and include such factors as cost; the belief that existing devices do not perform well in noise; and the fact that the demand for audiological services, even in developed countries, can be greater than the ability of the profession to provide them ().
In addition, there are those hearing-impaired individuals who have reliable access to hearing health care services, but who wish to be in control of their own fitting process, without having to rely on an audiologist to program and adjust the settings of their hearing aids. A recent survey by Kochkin (2007) that focused on obstacles to obtaining a hearing aid listed the top five characteristics that would increase the likelihood that a currently unaided individual would seek out a hearing aid. Two of the five characteristics were lower cost and the ability to self-fit or self-adjust a hearing aid. Forty percent of those surveyed indicated that a discount of US$500 would encourage them to purchase hearing aids, whereas 19% reported that the ability to self-fit or self-adjust their hearing aids would increase the likelihood of a hearing aid purchase (Kochkin, 2007).
A Self-Fitting Hearing Aid
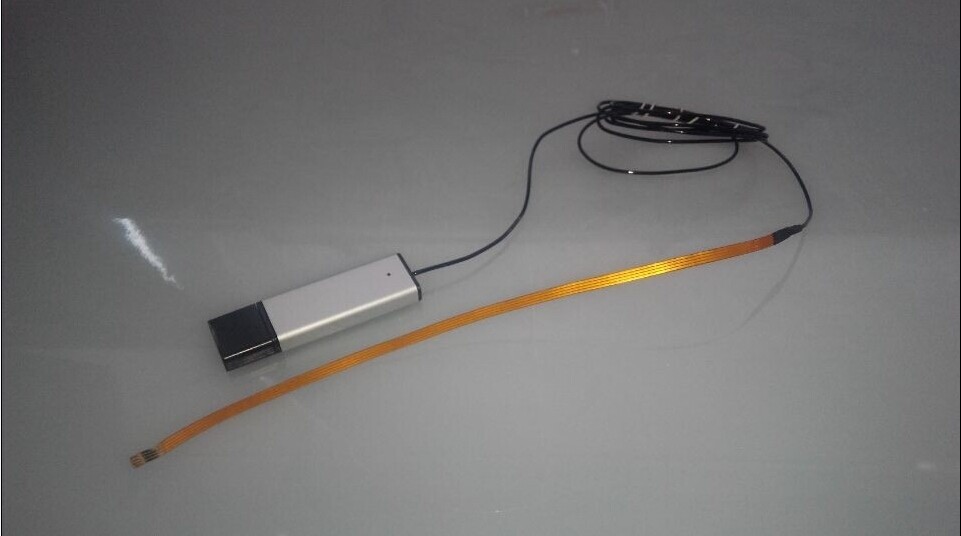
One possible solution for hearing-impaired individuals in both the developing and developed worlds is a “do-it-yourself” amplification device that can be fitted and managed entirely by the user, without the assistance of a hearing health care professional, the use of computer hardware, or access to a telephone or the internet. We refer to such a device as a “self-fitting” hearing aid. The concept of such a device is in the process of being evaluated at the National Acoustic Laboratories (NAL) in response to a growing global need for hearing health care services, particularly in developing nations and in remotely located, underserviced areas in developed countries.
The NAL vision of a self-fitting hearing aid is an amplification device that consists of a behind-the-ear (BTE) body and an instant-fit tip. The device contains a tone generator that may be activated either via an onboard button or with a remote control in order to start the process of an automated, in situ hearing threshold measurement. The same button is used by the hearing aid wearer to respond to the presented tones. An onboard prescriptive algorithm subsequently uses the measured thresholds as a basis for setting the hearing aid parameters (Figure 1). If the self-fitting hearing aid were equipped with a training algorithm and additional user controls, either on the device itself or on a remote control, the wearer would be able to further fine-tune the device in his or her everyday listening environments (Dillon et al., 2006). Briefly, we envision a training algorithm that concurrently collects and combines information about the acoustic characteristics of the user’s current environment and the user-selected settings in that environment. Over time, as sufficient data are accumulated, the hearing aid begins to anticipate the user’s preferred setting in a given listening environment and adjusts the hearing aid accordingly.
A model of the components of a self-fitting hearing aid
The concept of a self-fitting hearing aid is not new. In 1984, Köpke, Wiener, Maas, Eggert, and Götze patented the idea of a digital hearing aid that could present the user with internally generated tones in order to measure the user’s hearing thresholds, and then apply a transfer function to produce the prescribed hearing aid settings. This method of determining hearing aid settings very much describes the general concept of a self-fitting hearing aid. However, as far as we know, a device designed according to these principles has not yet been realized.
Whereas technological constraints may have prevented Köpke et al. and others of that era from realizing the kind of self-fitting hearing aid described in Figure 1, the prospect of producing a device that incorporates fully automated procedures for audiometric testing and hearing aid fitting is now very real. For example, many hearing aids are now equipped with tone generators (e.g. Intricon (2011), Widex, Siemens, and many others). These tone generators are primarily used to indicate changes to the volume level and program and as a low-battery indicator, although Widex (2011) makes use of this feature to provide harmonic tones that are designed to assist the user with relaxation and tinnitus relief (Kuk, Peeters, & Lau, 2010). The greater power and sophistication of digital hearing aid chipsets further make it feasible for the device to host a complex transfer function or prescriptive formula, and/or a training algorithm.
There are issues, however, that remain to be addressed before a self-fitting hearing aid is launched, some of which are explored and discussed in this issue of Trends in Amplification. For example, a factor that has yet to be investigated is the proportion of potential users who will be able to find an environment that is quiet enough for valid threshold measurements to be obtained. It may be possible for the device’s instructions to advise the user to move into a room or area in which no other sounds can be heard. Alternatively, the hearing aid microphone could be used to measure the ambient noise level, with a warning sound produced by the onboard tone generator whenever the masked thresholds are not better than the estimated masked threshold in that noise spectrum. The reliability and validity of in situ audiometric thresholds as measured with different styles of instant-fit tips are further discussed in Keidser et al. (2011) in this issue.
Commercial Alternatives
Currently, there are commercially available hearing aids that may be purchased and adjusted without visiting a hearing health care professional. Several of these devices could be considered “self-fitting” in that the wearer is in control of the fitting procedure. Additionally, a group of low-cost devices, produced specifically for the developing world, are currently available. Table 1 shows an overview of currently available hearing instruments that are distributed via nontraditional channels. The hearing aids summarized in the table can be broadly divided into two categories: (a) user-programmable devices, and (b) devices aimed specifically at clients in developing countries.
Table 1.
An overview of currently available hearing aids that are distributed through nontraditional channels
| Company | Website | Device characteristics | Price per device | User requirements |
|---|---|---|---|---|
| America Hears (2011) | http://www.americahears.com | digital; both custom and stock size products available | US$899-1,299 | computer, internet access, telephone, audiogram (optional: Virtual Office programming software, Freedom programming interface, and cables for self-programming; impressions for custom earmolds or shells) |
| Australia Hears (2011) | http://www.australiahears.com.au | digital; stock size products only | US$990-1,250 | computer, internet access (optional: audiogram; IHearYou programming software, AHPro3 programming interface, and cables for self-programming) |
| DIY Hearing Aids (2011) | http://www.diyhearingaids.com | digital; both custom and stock size products available | US$995-1,195 (optional: telecoil US$125, directional microphone US$125, custom earmold US$110) | computer, internet access, telephone, audiogram (optional: Virtual Technician programming software, eMini Tec programming interface, and cables for self-programming; impressions for custom earmolds or shells) |
| Godisa (2011) | http://www.godisa.org | digital; custom product only | unknown, but reportedly low cost | audiogram, impressions (optional: 2 cc coupler or real-ear measurement equipment) |
| HearSource (2011) | http://www.hearsource.com | digital; both custom and stock size products available | US$995 (optional: telecoil US$99, directional microphone US$99, custom earmold US$99) | computer, internet access, telephone, audiogram (optional: Virtual Technician programming software, eMini Tec programming interface, and cables for self-programming; impressions for custom earmolds or shells) |
| Solar Ear (2011) | http://www.solarear.com.br/solar | digital and analog; both custom and stock size products available | US$165-300; prices for some models unavailable | audiogram (optional: impressions for custom earmolds, 2 cc coupler or real-ear measurement equipment) |
User-Programmable Hearing Aids
The user-programmable devices, which include those sold by such companies as Australia Hears, America Hears, Hear Source, and DIY Hearing Aids, are digital hearing aids with such features as multichannel compression, adaptive feedback cancellation, and noise reduction and speech enhancement algorithms. Cost per device averages US$1,000, which is comparable to a low-cost traditionally fitted hearing aid.
In order to program and adjust the devices, a previous audiogram, a computer, internet access, fitting software, and/or a hardware interface between the computer and the hearing aids are required. The American companies (America Hears, Hear Source, and DIY Hearing Aids) require that the hearing aid candidate first contact a representative of the company for a telephone consultation. In order to comply with Food and Drug Administration (FDA) requirements, the candidate is required to submit an audiogram, a medical history and waiver form, and a Health Insurance Portability and Accountability Act (HIPAA) privacy policy form. America Hears runs an audiology center at which free hearing tests are offered; candidates who do not live near the center are advised to obtain a hearing test from a local audiologist. Hear Source and DIY Hearing Aids do not maintain brick-and-mortar hearing centers. Following the receipt of the necessary paperwork, the most appropriate hearing aid model is then chosen in consultation with the company representative. If a device requiring a custom earmold or shell is selected, the user must have ear impressions taken locally so the company can send them to the manufacturer. Ear impressions are not offered by any of the American companies discussed here. Hear Source and DIY Hearing Aids additionally offer a telephone appointment with a “coach” who can guide the user through the fine-tuning process and provide technical support. Due to the difference in Australian laws governing the provision of health-related products, Australian hearing aid candidates can order devices from Australia Hears with or without an audiogram. All devices purchased from these companies are delivered to the user preprogrammed. For those users who wish to undertake self-adjustments, fitting software, an interface box, and programming cables may be ordered in conjunction with the hearing aids. DIY Hearing Aids, America Hears, and Australia Hears charge an additional fee for these items.
The fitting software tends to be complex and sophisticated, resembling the fitting software used clinically by audiologists. For example, the fitting software offered by both Hear Source and DIY Hearing Aids includes an overall gain control with a 32 dB range, a 12-channel “equalizer” that allows gain adjustments at discrete frequencies from 0.2 kHz to 7.2 kHz, the ability to alter the compression threshold in four channels, a maximum power output (MPO) control, a slider to set the level of noise reduction, a toggle switch to activate or disable a feedback cancellation algorithm, and a choice of four microphone modes or input types (omnidirectional microphone, directional microphone, telecoil, direct audio input). Users can choose to implement any combination of these features in two programs. In the software, the hearing aid settings may be viewed as a gain curve or as an input/output function. Short tutorial videos that explain how to use many of the software functions are freely available on both websites and can also be found on YouTube. Both the software and the tutorials use such “clinical” vocabulary as frequency, intensity, decibel, and steady-state noise, which cannot be expected to be readily understood by the general population. In contrast, the IHearYou software offered by Australia Hears tends to be aimed more at troubleshooting problems that the user is experiencing in specific listening situations. For example, one screen asks the user to evaluate the quality of speech in background noise from a list of descriptors that include “clear,” “hollow or echoing,” and “muffled or dull.” On selecting an answer, the software presumably implements the corresponding changes to the gain/frequency response, compression parameters, and/or noise reduction algorithm.
Devices for Developing Countries
Devices geared to the developing world are currently produced and sold by Godisa and Solar Ear. Godisa is a charitable organization based in Botswana that produces and distributes several models of low-cost BTE hearing aids and a solar-powered battery recharger that is designed to accept a range of battery sizes (Brouillette, 2008; Godisa, 2011). Similarly, Solar Ear, located in Brazil, manufactures and distributes a range of analog and digital hearing aids, a solar-powered battery charger, and low-cost, long-life rechargeable hearing aid batteries (Solar Ear, 2011). The three digital hearing aid models offered by Solar Ear, which include two BTEs and one receiver-in-canal (RIC) device, feature two-channel wide dynamic range compression (WDRC) and a low-battery warning. The two BTE hearing aids, both for individuals with severe to profound hearing loss, also have telecoils, volume controls, and trimpots that allow alteration of MPO and high- and low-frequency gain. Specific information about Godisa devices could not be obtained as emails to the organization went unanswered. As of the date of the publication of this article, their website is no longer online.
As a secondary goal of these organizations is to provide meaningful employment for individuals who are deaf, these devices are assembled by members of the local deaf community. The technology is basic and adjustments to the devices’ settings, which may be made to achieve a match to a prescriptive target or to the user’s preferred level, are effected via screwdriver-adjustable trimpots. The method of device distribution is not clear, but it is likely that Godisa and Solar Ear hearing aids are fitted by local health personnel and/or audiologists associated with visiting aid agencies. None of these devices are designed to be self-adjusted by the wearer.
Other Nontraditional Hearing Aids
Figure 2 shows the two categories described above, as well as two other related device categories: (a) over-the-internet (OTI) hearing aids and (b) personal amplifiers. Although all currently available user-programmable hearing aids fall under the rubric of OTI devices, not all OTI devices are user programmable. The majority of OTI hearing aids are preprogrammed by the manufacturer or distributor according to a user-supplied audiogram before being dispensed by mail. As these devices require an audiogram for programming, the hearing aid candidate still needs to visit a hearing health care professional to obtain a hearing test. Personal amplifiers, some of which are available OTI, are similar to hearing aids in that they provide some degree of amplification. However, any adjustments that may be made to their gain/output are not frequency-specific, and thus these devices cannot be matched to the user’s individual audiometric thresholds. Their manufacture and sale are often not controlled by government regulatory bodies, and as such, do not meet sufficient quality and safety standards to be marketed as hearing aids or medical devices. subjected 11 low- and mid-range over-the-counter (OTC) hearing devices, all of which are available OTI, to a battery of electroacoustic tests. These tests included measurements of full-on gain, total harmonic distortion, equivalent input noise (EIN), frequency range, battery life, and the presence of high-frequency peaks. The suitability of each device for three audiometric configurations relative to the National Acoustic Laboratories-Revised (NAL-R; ) prescriptive formula was also investigated. The results showed that the low-range devices were inadequate, with high levels of EIN, little to no high-frequency gain, peaky frequency responses, and high battery drain displayed by some or all of the devices. The potential for these devices to damage users’ residual hearing due to the high output levels measured in the low-range devices was also highlighted by the authors.
Unlike a self-fitting hearing aid, which is designed to be entirely self-contained, all currently available nontraditional hearing aids and self-tests of hearing require either additional equipment and/or access to a hearing health care professional
The fifth and final category shown in Figure 2 encompasses self-tests of hearing. Currently, all self-tests of hearing are computer-, telephone-, and/or questionnaire-based. None of these test methods provides the person being tested with reliable, frequency-specific thresholds to which a validated prescriptive algorithm can be applied to yield hearing aid settings. There are currently no self-tests of hearing available in a hearing aid or other wearable device that does not require the attachment of an additional programming unit (e.g., Ludvigsen & Topholm, 1997), or a computer.
The self-fitting hearing aid concept under investigation at NAL is designed to incorporate aspects of three categories described in Figure 2 into a single device: (a) a self-test of the user’s hearing, (b) user programmability, and (c) suitability for developing countries. Consequently, the self-fitting hearing aid concept currently being explored at NAL aims to be a unique solution that can be fitted and managed entirely by the user, without the need for access to a hearing health care professional or additional equipment.
Programmable Digital Hearing Aids Prices
Potential Advantages and Disadvantages
As with any new invention, there are both possible benefits and drawbacks to the introduction of a self-fitting hearing aid into the market. An anticipated advantage of a self-fitting hearing aid is the expected lower financial cost. As discussed earlier in this article, the price of a hearing aid in a developing country is often prohibitively expensive relative to average household income (Brouillette, 2008). In the case of a self-fitting hearing aid, the lack of need for a professional hearing health care provider, as well as the reduced need for travel to and from the clinic, is likely to represent a significant cost savings for the user. This advantage could also be attractive to hearing aid candidates in developed countries.
If trainability is an incorporated feature in the self-fitting device, the ability of the user to undertake the fine-tuning process in response to real-world listening situations could be an advantage. Hearing aid fittings and subsequent fine-tuning adjustments are traditionally conducted in a quiet room with a single sound source and little to no background noise, an acoustic environment that differs markedly to the average user’s everyday listening situations. Although it is important to ensure that the hearing aid operates appropriately in this kind of “best case” environment, users may not necessarily find the initial setting preferable as they step out of the clinic and into a busy street. To rectify this problem, some proprietary fitting software packages include a comprehensive library of sounds, accompanied by still pictures or virtual scenes, that replicate everyday listening situations (e.g., Howes & Olson, 2006; Meskan & Robinson, 2000). At present, however, there are limitations to the degree to which an acoustic environment can be accurately reproduced, especially when constrained by the limited number of loudspeakers typically found in an audiology clinic (Guastavino, Katz, Polack, Levitin, & Dubois, 2005). Additionally, the unique range of the user’s most commonly encountered listening situations may not be adequately represented among the sound library. In contrast, a self-fitting hearing aid would allow users to fine-tune and personalize their settings in response to their own individual listening environments.
A further anticipated advantage of a self-fitting and/or trainable hearing aid is the increased feeling of psychological ownership that such a device is expected to confer on the user. The concept of psychological ownership refers to the internalized feelings of possession we have toward other entities or “targets,” which may include objects, ideas, or even other people. Individuals incorporate ownership targets into their own self-identity, using them to help define who they are (Pierce, Kostova, & Dirks, 2003). Although psychological ownership has not been widely researched in relation to health care, Karnilowicz (2010) argues that the concept can usefully be extended to include chronic health conditions and their associated treatments. For example, an individual may feel a sense of ownership toward his or her hearing loss and hearing aids, and therefore that they constitute part of his or her identity.
Psychological ownership and self-identity are intrinsically bound up with the notion of control. Pierce et al. (2003) state that the strength of psychological ownership (and, hence, the extent to which it is integrated into the individual’s self-identity) is strongly influenced by the degree of control the individual is able to exercise over his or her ownership targets. In the context of current research into management of chronic health conditions, this is very much in line with the wealth of studies demonstrating that the role of the patient as an active collaborator in, rather than the passive recipient of, the treatment of his or her own chronic health condition leads to improved adherence and better outcomes (e.g., ; ; ).
Control over one’s ownership targets is influenced by a range of factors, the most important of which is self-creation (Pierce et al., 2003). That is, individuals will experience a greater sense of ownership of, and control over, something they invest in creating themselves. This will arguably be the case for users of a self-fitting hearing aid, as unlike a hearing aid fitted by a professional, the device requires a substantial investment of effort and time by the end user. This advantage may apply more to users in developed countries who are able to choose a self-fitting hearing aid from a range of hearing health care options, as opposed to those in the developing world whose choices are limited or nonexistent.
Depending on one’s perspective, the fact that a self-fitting hearing aid does not require direct input from a hearing health care professional may be seen either as an advantage or a disadvantage. From the point of view of some end users, this freedom may be viewed as an advantage. Elberling and Hansen (1999) have suggested that three conditions must be met in order for a traditional hearing aid to be successfully fine-tuned: (a) a clear description of the problem by the user, (b) correct interpretation of the problem by the hearing health care professional, and (c) the translation of the problem into appropriate changes to the hearing aid’s electroacoustic characteristics. Even if only one of these conditions is not fulfilled, the fine-tuning process is unlikely to yield the preferred response. Although key words associated with specific auditory percepts have been identified (Nelson, 2001) and flow charts have been developed to aid the hearing health care professional in interpreting a client’s complaints (Kuk, 1999), the second and third conditions remain difficult to meet in all cases. A self-fitting hearing aid, however, allows users to act directly on and experiment with their own settings, without relying on their ability to translate perceptions into words or a professional’s ability to translate words into adjustments.
A potential disadvantage of a self-fitting hearing aid is the risk of an audiologically inappropriate fitting. Identifying the presence of a conductive or mixed hearing loss is a critical step prior to hearing aid fitting, as many pathologies of the outer or middle ear can be treated medically or should be investigated prior to fitting with amplification (Silman & Silverman, 1997). In the lead-up to a traditional hearing aid fitting, such contraindications are often able to be discerned through a combination of otoscopy and audiometry. For example, impacted wax in the ear canal can be detected with an otoscope, whereas air- and bone-conduction thresholds on the audiogram will distinguish between sensorineural and conductive sites of lesion. In the case of the self-fitting hearing aid, however, otoscopy cannot be performed, as a person cannot easily look into one’s own ear canal. Such other contraindications to a hearing aid fitting as a sudden or rapidly progressing hearing loss, otalgia, a physical malformation of the ear, or active infection may also, if overlooked, result in poor fitting outcomes for the user. Other issues that may arise after the fitting include the selection of inappropriately high levels of gain and output, which may lead to temporary or permanent threshold shift, particularly among users with severe and profound hearing loss (). The safety of a self-fitting hearing aid will depend on how well the device can identify the presence of conductive and asymmetrical hearing losses, and how accurately it is able to measure hearing thresholds and to prescribe an appropriate gain/frequency response, compression parameters, and MPO. Such issues require further investigation.
Home Programmable Hearing Aids
The threat that the self-fitting hearing aid could pose to the livelihood of hearing health care professionals depends, in developed countries, on the extent to which the device is taken up by existing hearing aid users versus individuals who are currently unaided. If the former situation occurs, then the impact on the profession will depend on the overall supply and demand for audiological services. It is important to recognize, however, that many people will continue to need considerable assistance from clinicians for diagnosis, motivational counseling, and/or instructional counseling in device usage and listening tactics. Although the candidacy criteria for a self-fitting hearing aid are unknown at present, infants, young children, and individuals with cognitive and/or fine motor difficulties are examples of groups who are unlikely to be suitable candidates for a self-fitting device. Such populations will continue to require direct clinical interaction with a hearing health care professional.
Practical issues that may present a challenge include finding a suitable instant-fit ear tip and ensuring a reliable battery supply to users of the self-fitting hearing aid. Instant-fit tips (and even custom-made earmolds) have a shorter lifespan than the amplification devices to which they are attached. Although extra tips could be provided with the self-fitting hearing aid, a long-term solution is needed that will allow users in remote and developing parts of the world to access affordable replacement tips. A similar problem exists for batteries. Rechargeable and solar-powered batteries are an obvious solution, and are currently being produced by such organizations as Solar Ear. However, even these products have a limited lifespan. Electrically powered battery chargers would not suit populations living without electricity, while solar-powered devices would be impractical for those dwelling in areas with little daylight for several months of the year. If the self-fitting hearing aid is to be realized, a carefully thought-out distribution model is required to ensure that those who obtain the device can continue to use it. In developing countries, it is also critical that those individuals with severe hearing loss, for whom instant-fit tips may not be suitable due to their high gain requirements, are catered for through the provision of suitable custom earmolds.
Considerations for Future Investigations
As pointed out earlier in this article, the self-fitting hearing aid concept relies on the capability of the device to achieve reliable and valid in situ thresholds using an automated procedure that is fully administered by the hearing aid user. Several studies have demonstrated that automated audiometry is as reliable and valid as manual audiometry (e.g., ; ), and a recent study also proved the reliability and validity of in situ audiometry, provided that transducer-specific real-ear-to-dial difference (REDD) values are applied to the threshold measurements to compensate for low-frequency leakage (). These studies are reviewed in more detail in an accompanying article (Keidser et al., in press), which also addresses such issues as the detection of asymmetry and conductive loss, two possible contraindications to a conventional hearing aid fitting. To our knowledge, there exists no hearing aid with an onboard tone generator that can be activated by the user to complete an audiometric test. When a device with such a feature becomes available, the ability of a layperson to follow and understand a set of instructions to complete automated audiometry, and the reliability and validity of the resulting measurements, will need to be verified. Such research could include investigations into the levels of ambient noise in the environments that users of the device typically select for performing audiometric testing.
Unless it is possible to design a one-size-fits-all device, a candidate for the self-fitting hearing aid will likely need to assemble several hearing aid components prior to performing automated in situ audiometry. Specifically, we expect that the user will need to select appropriate tube and instant-fit tip sizes from a range of different sizes, connect them to the body of a hearing aid, insert a battery into the assembled device, and learn how to insert the aid into the ear. In a conventional hearing aid fitting, such tasks are left to the hearing aid provider, who also has experience in determining whether the aid fits well in the person’s ear. Again, a successful outcome here is likely to depend on the instructions provided. This aspect has been explored in a group of older, urban-dwelling, hearing-impaired adults living in a developed country (Australia), and the results are presented in an accompanying article (). The study found that health literacy, or the ability to read and understand health-related text, was an important predictor of the outcome, with participants who had a higher level of health literacy better able to complete the tasks accurately and independently. This result clearly points toward the importance of supplying simple instructions with the self-fitting hearing aid. Another accompanying article in this issue () explains how health literacy differs from general literacy, and presents and discusses the steps involved in developing written health care material using best practice design principles. The steps are further illustrated through the development of the instructions for assembling and inserting a hearing aid that were used in the ) study. From these investigations, it becomes clear that future studies must focus on devising clear instructions for how to assemble, self-fit, and fine-tune the hearing aid.
We believe that the primary market for the self-fitting hearing aid should be developing countries that lack an audiological infrastructure. Therefore, when developing instructions for use of the device, the high rate of illiteracy in such areas should be considered and the efficacy of the instructions verified in the target population. More information about the disadvantages currently faced by hearing-impaired people living in developing countries and how innovative technology could make a difference in these areas are discussed in an accompanying article by McPherson (in press). In this article, McPherson highlights the lack of research into how to match amplification technology with the need in developing countries for affordable and appropriate devices.
Perception of the self-fitting concept has been gauged among urban-dwelling, hearing-impaired adults in a developed country (). Overall, perception of the concept among this population sample was positive. Interestingly, although self-adjustment, convenience, and independence were the most cited advantages, the most cited disadvantage was a personal preference for professional guidance. This outcome was measured in a population that has a choice of hearing health care services, and is not likely to be directly applicable to hearing-impaired individuals in a developing country. It would therefore be beneficial to survey residents of a developing country to determine whether the self-fitting hearing aid is an appropriate and desirable solution, or whether this population would prefer an investment in building local centers at which hearing services are provided, either by trained professionals or through the use of teleaudiology.
Before a self-fitting hearing aid could be made available in either developing or developed countries, a thorough evaluation must be performed to establish that the outcome of using a self-fitting hearing aid is at least as good as the outcome achieved with a professional hearing aid fitting. On a somewhat related topic, Wong (in press) looks at the current research on three elements related to a self-fitting hearing aid and reviews them using evidence-based principles: the performance of in situ threshold measurements, the ability of hearing aid users to reliably select their preferred responses in different listening environments and associated outcomes, and the ability of older adults to assemble and use a hearing aid. None of these research questions were answered with high quality evidence and some specific questions have yet to be addressed, suggesting that there is scope for more investigations in all three areas.
Summary
This article introduced the concept of a “do-it-yourself” amplification device that requires no access to further instrumentation and that can be managed, fitted, and fine-tuned entirely by the user, either independently or with the assistance of another layperson. Such a device would offer people who live in developing countries and in geographically remote areas increased access to hearing rehabilitation. We further argue that a proportion of hearing-impaired people who already have reliable access to audiological services, but who wish to play a greater role in the fitting and fine-tuning process, could also benefit from the availability of such a device. The anticipated advantages of a self-fitting hearing aid include the expected lower cost of such a device, the ability to fine-tune the device’s settings in response to real-world listening situations, an increased sense of psychological ownership, and the freedom from dependence on a hearing health care professional, while the possible disadvantages include the risk of an audiologically inappropriate fitting, the risk of aid-induced hearing loss if excessively high gain and output levels are selected, and the high level of cognitive functioning that is likely to be required to carry out the self-fitting procedure. The distribution model of a self-fitting hearing aid, with a particular focus on the supply of replacement instant-fit tips and batteries, presents a challenge that must be carefully addressed.
Footnotes
Authors’ Note: Portions of this article were presented at the 30th International Congress of Audiology in São Paulo, Brazil, April 2010.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed the receipt of the following financial support for the research, authorship, and/or publication of this article: Funding for this study was provided by the HEARing Cooperative Research Centre, Melbourne, Australia.
References
- America Hears. (2011). Programming and adjustment options. Retrieved from http://www.americahears.com/Products/VirtualOffice.shtml
- Australia Hears. (2011). Our hearing aid prices and accessories. Retrieved from https://www.australiahears.com.au/Online-Store.aspx
- Bento R., Penteado S. (2010). Designing of a digital behind-the-ear hearing aid to meet the World Health Organization requirements. Trends in Amplification, 14, 64-72 [PMC free article] [PubMed] [Google Scholar]
- Brouillette R. (2008). Rehabilitation of hearing loss: challenges and opportunities in developing countries. In McPherson B., Brouillette R., editors. (Eds.), Audiology in developing countries (pp. 141-154). New York, NY: Nova Science [Google Scholar]
- Byrne D., Dillon H. (1986). The National Acoustic Laboratories’ new procedure for selecting the gain and frequency response of a hearing aid. Ear and Hearing, 7, 257-265 [PubMed] [Google Scholar]
- Callaway S. L., Punch J. L. (2008). An electroacoustic analysis of over-the-counter hearing aids. American Journal of Audiology, 17, 14-24 [PubMed] [Google Scholar]
- Caposecco A., Hickson L., Meyer C. (2011). Assembly and insertion of a self-fitting hearing aid: Design of effective instruction materials. Trends in Amplification, 15 (4), 184-195 [PMC free article] [PubMed] [Google Scholar]
- Choi J., Lee H., Park C., Oh S., Park K. (2007). PC based tele-audiometry. Telemedicine and eHealth, 13(5), 501-508 [PubMed] [Google Scholar]
- Convery E., Keidser G., Hartley L. (2011a). Perception of a self-fitting hearing aid among urban-dwelling hearing-impaired adults in a developed country. Trends in Amplification, 15 (4), 175-183 [PMC free article] [PubMed] [Google Scholar]
- Convery E., Keidser G., Hartley L., Caposecco A., Hickson L., Meyer C. (2011b). Management of Hearing Aid Assembly by Urban-Dwelling Hearing-Impaired Adults in a Developed Country: Implications for a Self-Fitting Hearing Aid. Trends in Amplification, 15(4), 196-208 [PMC free article] [PubMed] [Google Scholar]
- Dillon H. (in press). Hearing aids (2nd ed.). Sydney, Australia: Boomerang Press [Google Scholar]
- Dillon H., Zakis J. A., McDermott H., Keidser G., Dreschler W., Convery E. (2006). The trainable hearing aid: what will it do for clients and clinicians?Hearing Journal, 59, 30-36 [Google Scholar]
- DIY Hearing Aids. (2011). Hearing aid product list and order page. Retrieved from http://www.diyhearingaids.com/digital-hearing-aid-products
- Elberling C., Hansen K. V. (1999). Hearing instruments: interaction with user preference. In Rasmussen A. N., Osterhammel P. A., Andersen T., Poulsen T., editors. (Eds.), Auditory models and non-linear hearing instruments. Proceedings of the18th Danavox Symposium (pp 341-357). Copenhagen, Denmark: Holmens Trykkeri [Google Scholar]
- Ferrari D. V. (2005). Remote programming and verification as a mean to improve quality of hearing and fitting. In Rasmussen A. N., Poulsen T., Andersen T., Larsen C. B., editors. (Eds.) Hearing aid fitting. Proceedings of the 21st Danavox Symposium (pp 531-543). Aalborg, Denmark: Centertryk [Google Scholar]
- Gardetto N. J. (2011). Self-management in heart failure: Where have we been and where should we go?Journal of Multidisciplinary Healthcare, 4, 39-51 [PMC free article] [PubMed] [Google Scholar]
- Godisa. (2011). About Godisa: Technologies for the developing world. Retrieved from http://www.godisa.org/about.html
- Goulios H., Patuzzi R. (2008). Education and practice of audiology internationally: Affordable and sustainable education models for developing countries. In McPherson B., Brouillette R., editors. (Eds.), Audiology in developing countries (pp. 51-74). New York, NY: Nova Science [Google Scholar]
- Guastavino C., Katz B. F. G., Polack J. D., Levitin D. J., Dubois D. (2005). Ecological validity of soundscape reproduction. Acustica, 91, 333-341 [Google Scholar]
- HearSource. (2011). Hearing aid programming. Retrieved from http://www.hearsource.com/hearing_aid_software.html
- Ho A. T. P., Hildreth A. J., Lindsey L. (2009). Computer-based audiometry versus manual audiometry. Otology & Neurotology, 30, 876-883 [PubMed] [Google Scholar]
- Howes C., Olson L. (2006). The role of virtual reality in hearing instrument fittings. Hearing Review, 13(5), 60-63 [Google Scholar]
- Intricon. (2011). The all-new Overtus™. Retrieved from http://intricon.com/products/hearing-health/digital-amplifiers/overtus/
- Karnilowicz B. (2011). Identity and psychological ownership in chronic illness and disease state. European Journal of Cancer Care, 20, 276-282 [PMC free article] [PubMed] [Google Scholar]
- Keidser G., Dillon H., Zhou D., O’Brien A., Carter L., Yeend I., Hartley L. (in press). Expected reliability and validity of thresholds measured automated and in situ. Trends in Amplification
- Kochkin S. (2005). MarkeTrak VII: Consumer satisfaction with hearing instruments in the digital age. Hearing Journal, 58, 30-43 [Google Scholar]
- Kochkin S. (2007). MarkeTrak VII: Obstacles to adult non-user adoption of hearing aids. Hearing Journal, 60, 24-51 [Google Scholar]
- Köpke W., Wiener P., Maas R., Eggert A., Götze G. W. (1984). Digital hearing aid and method. U.S. Patent No. 4,471,171September11, 1984
- Kralik D., Koch T., Price K., Howard N. (2004). Chronic illness self-management: taking action to create order. Journal of Clinical Nursing, 13, 259-267 [PubMed] [Google Scholar]
- Krumm M., Huffman T., Dick K., Klich R. (2008). Telemedicine for audiology screening of infants. Journal of Telemedicine and Telecare, 14, 102-104 [PubMed] [Google Scholar]
- Kuk F. K. (1999). How flow charts can help you troubleshoot hearing aid problems. Hearing Journal, 52, 46, 48,-49, 52 [Google Scholar]
- Kuk F., Peeters H., Lau C. (2010). The efficacy of fractal music employed in hearing aids for tinnitus management. Hearing Review, 17(10), 32-42 [Google Scholar]
- Laplante-Levesque A., Pichora-Fuller K. M., Gagne J. P. (2006). Providing an internet-based audiological counselling programme to new hearing aid users: A qualitative study. International Journal of Audiology, 45, 697-706 [PubMed] [Google Scholar]
- Ludvigsen C., Topholm J. (1997). Fitting a wide range compression hearing instrument using real ear threshold data: a new strategy. High Performance Hearing Solutions, 2, 37-39 [Google Scholar]
- Macrae J. (1991). Prediction of deterioration in hearing due to hearing aid use. Journal of Speech and Hearing Research, 34, 661-670 [PubMed] [Google Scholar]
- Margolis R. H., Glasberg B. R., Creeke S., Moore B. C. J. (2010). AMTAS®: Automated method for testing auditory sensitivity: Validation studies. International Journal of Audiology, 49(3), 185-194 [PubMed] [Google Scholar]
- Mayor V. (2006). Long-term conditions. 3: Being an expert patient. British Journal of Community Nursing, 11, 59-63 [PubMed] [Google Scholar]
- McPherson B. (2008). Audiology: a developing country context. In McPherson B., Brouillette R., editors. (Eds.), Audiology in developing countries (pp. 5-20). New York, NY: Nova Science [Google Scholar]
- McPherson B. (2011). Innovative technology in hearing instruments: Matching needs in the developing world. Trends in Amplification, 15(4), 209-1214 [PMC free article] [PubMed] [Google Scholar]
- Meskan M. E., Robinson J. L. (2000). A patient-focused approach to fitting hearing instruments. Hearing Review, 7(12), 52-55 [Google Scholar]
- Nelson J. A. (2001). Fine tuning multi-channel compression hearing instruments. Hearing Review, 8, 30, 32, 34,-35, 58 [Google Scholar]
- O’Brien A., Keidser G., Yeend I., Hartley L., Dillon H. (2010). Validity and reliability of in situ air conduction thresholds measured through hearing aids coupled to closed and open instant-fit tips. International Journal of Audiology, 49, 868-876 [PubMed] [Google Scholar]
- Parving A., Christensen B. (2004). Clinical trial of a low-cost, solar-powered hearing aid. Acta Oto-Laryngologica, 124, 416-429 [PubMed] [Google Scholar]
- Pearce W., Ching T. Y. C., Dillon H. (2009). A pilot investigation into the provision of hearing services using tele-audiology to remote areas. Australian and New Zealand Journal of Audiology, 31(2), 96-100 [Google Scholar]
- Pierce J. L., Kostova T., Dirks K. T. (2003). The state of psychological ownership: Integrating and extending a century of research. Review of General Psychology, 7, 84-107 [Google Scholar]
- Silman S., Silverman C. A. (1997). Auditory diagnosis: Principles and applications. San Diego, CA: Singular [Google Scholar]
- Smith A. W. (2008). Demographics of hearing loss in developing countries. In McPherson B., Brouillette R., editors. (Eds.), Audiology in developing countries (pp. 21-50). New York, NY: Nova Science [Google Scholar]
- Solar Ear. (2011). Welcome to solar ear: The problem, the solution, the impact. Retrieved from http://www.solarear.com.br/solar/
- Swanepoel D., Clark J. L., Koekemoer D., Hall J. W., Krumm M., Ferrari D., McPherson B., Olusanya B., Mars M., Barajas J. (2010). Telehealth in audiology: The need and potential to reach underserved communities. International Journal of Audiology, 49, 195-202 [PubMed] [Google Scholar]
- United Nations Office of the High Representative for the Least Developed Countries, Landlocked Developing Countries, and the Small Island Developing States. (2011). About LDCs, LLDCs, and SIDS. Retrieved from http://www.unohrlls.org/
- Wesendahl T. (2003). Hearing aid fitting: Application of telemedicine in audiology. International Tinnitus Journal, 9(1), 56-58 [PubMed] [Google Scholar]
- Widex. (2011). Mind440 key features. Retrieved from http://www.widex.pro/en/products/series/clear440/
- Wong L. L. N. (2011). Evidence on self-fitting hearing aids. Trends in Amplification, 15(4), 215-225 [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2004). Guidelines for hearing aids and services for developing countries (2nd ed.). Geneva, Switzerland: World Health Organization; Retrieved from www.who.int/pbd/deafness/en/hearing_aid_guide_en.pdf[Google Scholar]